Anthem Blue Cross 2002 Annual Report Download - page 87
Download and view the complete annual report
Please find page 87 of the 2002 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
NOTES
to Consolidated Financial Statements (Continued)
82 Anthem, Inc. 2002 Annual Report
Insurance Company (“Alliance”), under a contract
between Alliance and the United States Department of
Defense. Under that contract, Alliance managed and
administered the TRICARE Managed Care Support
Program for military families from May 1, 1998 through
May 31, 2001, at which time the TRICARE operations
were sold. There was no call on the guarantee for the
period from May 1, 1998 to May 31, 2001 (which period
is now “closed”).
Vulnerability from Concentrations
Financial instruments that potentially subject the
Company to concentrations of credit risk consist primarily
of investment securities and premium receivables. All
investment securities are managed by professional invest-
ment managers within policies authorized by the Board of
Directors. Such policies limit the amounts that may be
invested in any one issuer and prescribe certain investee
company criteria. Concentrations of credit risk with
respect to premium receivables are limited due to the large
number of employer groups that constitute the Company’s
customer base in the geographic regions in which it con-
ducts business. As of December 31, 2002, there were no
significant concentrations of financial instruments in a
single investee, industry or geographic location.
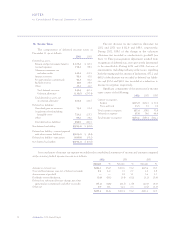
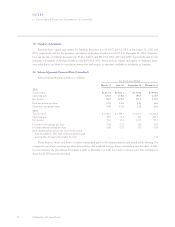
18. Segment Information
The Company’s principal reportable segments are
strategic business units primarily delineated by geographic
areas that essentially offer similar insurance products and
services. They are managed separately because each geo-
graphic region has unique market, regulatory and health
care delivery characteristics. The geographic regions are:
the Midwest region, which operates primarily in Indiana,
Kentucky and Ohio; the East region, which operates pri-
marily in Connecticut, New Hampshire and Maine; the
West region, which operates in Colorado and Nevada;
and the Southeast region, which operates in Virginia,
excluding the Northern Virginia suburbs of Washington,
D.C. BCBS-ME is included in the East segment since its
acquisition date of June 5, 2000. The Southeast region
was added with the July 31, 2002 acquisition of Trigon.
In addition to its four principal reportable geographic
segments, the Company operates a Specialty segment,
which includes business units providing group life and
disability insurance benefits, pharmacy benefit manage-
ment, dental and vision administration services and
behavioral health benefits services. Various ancillary
business units (reported with the Other segment) consist
primarily of AdminaStar Federal which administers
Medicare programs in Indiana, Illinois, Kentucky and
Ohio and Anthem Alliance, which provided health care
benefits and administration in nine states for the
Department of Defense’s TRICARE Program for military
families. The TRICARE operations were sold on May 31,
2001. The Other segment also includes intersegment
revenue and expense eliminations and corporate expenses
not allocated to reportable segments.
Through its participation in the Federal Employee
Program, Medicare, Medicare at Risk, and TRICARE
Program, the Company generated approximately 18%,
20% and 22% of its total consolidated revenues from
agencies of the U.S. government for the years ended
December 31, 2002, 2001 and 2000, respectively.
The Company defines operating revenues to include
premium income, administrative fees and other revenues.
Operating revenues are derived from premiums and fees
received primarily from the sale and administration of
health benefit products. Operating expenses are com-
prised of benefit and administrative expenses. The
Company calculates operating gain or loss as operating
revenue less operating expenses.
The accounting policies of the segments are the
same as those described in the summary of significant
accounting policies except that certain shared adminis-
trative expenses for each segment are recognized on a pro
rata allocated basis, which in aggregate approximates the
consolidated expense. Any difference between the allo-
cated expenses and actual consolidated expense is
included in other expenses not allocated to reportable
segments. Intersegment sales and expenses are recorded at
cost, and eliminated in the consolidated financial state-
ments. The Company evaluates performance of the
reportable segments based on operating gain or loss as
defined above. The Company evaluates investment
income, interest expense, amortization expense and
income taxes, and asset and liability details on a consoli-
dated basis as these items are managed in a corporate
shared service environment and are not the responsibility
of segment operating management.