Anthem Blue Cross 2002 Annual Report Download - page 43
Download and view the complete annual report
Please find page 43 of the 2002 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
MANAGEMENT’S DISCUSSION AND ANALYSIS
of Financial Condition and Results of Operations (Continued)
38 Anthem, Inc. 2002 Annual Report
Operating gain increased $54.6 million to $74.7 mil-
lion in 2002, primarily due to improved underwriting
results in our Local Large Group fully-insured and Small
Group businesses. Also contributing to the improvement
was $10.9 million in favorable prior year reserve releases
recorded during the third quarter of 2002. These reserve
releases were offset by a $10.1 million reserve increase
for case specific reserves incurred during the normal
course of business.
Membership increased 67,000, or 9%, primarily due
to increased BlueCard activity and higher sales in our
Individual business.
Southeast
Our Southeast segment is comprised of health benefit
and related business for members in Virginia, excluding
the Northern Virginia suburbs of Washington D.C. Our
Southeast segment’s summarized results of operations for
the five months ended December 31, 2002 are as follows:
Five Months
Ended December 31, 2002
($ in Millions)
Operating Revenue $1,467.9
Operating Gain $ 116.0
Operating Margin 7.9%
Membership (in 000s) 2,549
Our Southeast segment was established with the
acquisition of Trigon on July 31, 2002. Results of operations
for this segment have been included in our consolidated
financial statements from August 1, 2002 forward. These
five months of operating results may not be sustainable or
indicative of future performance, as we are in the early
stages of transitioning business practices and policies that
will govern our Southeast segment’s operations. Our inte-
gration activities remain on schedule, and we expect to
achieve $40.0 million to $50.0 million of synergies in
2003 and at least $75.0 million by 2004. We captured
approximately $11.0 million of synergies in 2002, prima-
rily related to corporate overhead and information tech-
nology cost savings.
Specialty
Our Specialty segment includes our group life and
disability insurance benefits, pharmacy benefit manage-
ment, dental and vision administration services and
behavioral health benefits services. During the third
quarter of 2002, we sold our third party occupational
health services businesses, the operating results of which
were not material to the earnings of this segment or our
consolidated results. On June 1, 2002, we acquired cer-
tain assets of PRO Behavioral Health, or PRO, a Denver,
Colorado-based behavioral health company in order to
broaden our specialty product offerings. Results from this
acquisition are included from that date forward and are
not material to the operating revenue or operating gain of
this segment in the year ended December 31, 2002.
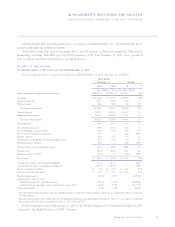
Our Specialty segment’s summarized results of opera-
tions for the years ended December 31, 2002 and 2001
are as follows:
Years Ended
December 31
2002 2001 $ Change % Change
($ in Millions)
Operating Revenue $523.5 $396.1 $127.4 32%
Operating Gain $ 50.7 $ 32.9 $ 17.8 54%
Operating Margin 9.7% 8.3% 140 bp
Operating revenue increased $127.4 million, or
32%, primarily due to increased mail-order prescription
volume at APM. APM launched mail-order campaigns to
inform members of the benefits and convenience of using
APM’s mail-order pharmacy option for maintenance
drugs. In addition, APM increased its penetration of our
health benefits members. APM implemented its phar-
macy benefit programs in our West segment and in Maine
during the first six months of 2001. Excluding the impact
of our TRICARE operations, mail-service prescription
volume increased 29% and retail prescription volume
increased 10%.