Anthem Blue Cross 2002 Annual Report Download - page 39
Download and view the complete annual report
Please find page 39 of the 2002 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
MANAGEMENT’S DISCUSSION AND ANALYSIS
of Financial Condition and Results of Operations (Continued)
34 Anthem, Inc. 2002 Annual Report
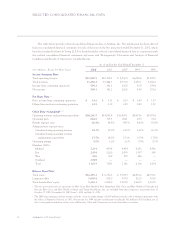
On a same-store basis, other revenue, which is com-
prised principally of co-pays and deductibles associated
with Anthem Prescription Management’s, or APM’s, sale
of mail-order drugs, increased $24.2 million, or 42%.
Mail-order revenues increased primarily due to additional
volume. APM launched mail conversion campaigns to
inform members of the benefits and convenience of using
APM’s mail-order pharmacy option during 2002. In addi-
tion, APM increased its penetration of our health bene-
fits membership, with a resulting larger enrollment base
and therefore greater demand for mail-order service.
Benefit expense increased $2,024.7 million, or 26%,
in 2002. On a same-store basis, benefit expense increased
$1,132.7 million, or 15%, primarily due to increased cost of
care trends and higher average membership. Higher costs
of care were driven primarily by higher costs in professional
services and outpatient services. Our benefit expense ratio
decreased 210 basis points from 84.5% in 2001 to 82.4% in
2002 due partly to the sale of our TRICARE operations in
2001 and the impact of our Trigon acquisition in 2002. On
a same-store basis, our benefit expense ratio decreased
160 basis points from 84.2% in 2001 to 82.6% in 2002,
primarily due to lower than anticipated medical costs in
all of our business segments. Our 2002 benefit expense
was also reduced by favorable developments of reserves
reported as of December 31, 2001.
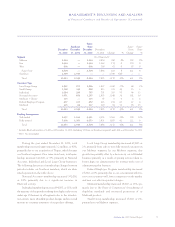
The following discussion summarizes our aggregate
cost of care trends for the 12-month period ended
December 31, 2002, for our Local Large Group and Small
Group fully-insured businesses only. Our cost of care
trends are calculated by comparing per member per month
claim costs for which Anthem is responsible, which
excludes member co-payments and deductibles. Our aggre-
gate cost of care trend including the impact of our Trigon
acquisition for the entire rolling 12-month periods, includ-
ing periods prior to July 31, 2002, was approximately
12%. Our aggregate cost of care trend excluding the
impact of our Trigon acquisition was approximately one-
half percentage point higher, driven primarily by pro-
fessional services costs and outpatient services costs,
weighted as a percentage of cost of care expense.
Cost increases for professional services were approxi-
mately 12% including the impact of our Trigon acquisi-
tion for the entire rolling 12-month periods, including
periods prior to July 31, 2002. Excluding the impact of
our Trigon acquisition, our professional services trend was
approximately one and one-half percentage points higher.
This trend is due to both higher utilization and higher
unit costs. Utilization increases were driven primarily by
increases in physician office visits, radiology procedures
such as Magnetic Resonance Imaging procedures, or
MRIs, Positron Emission Tomography procedures, or PET
scans, and laboratory procedures. Unit cost increases were
driven primarily by increases in physician fee reimburse-
ment schedules. In response to increasing professional
services costs, we continue to work with our providers
through education and contracting to ensure that our
members receive the most appropriate care at the proper
time in the appropriate clinical setting.
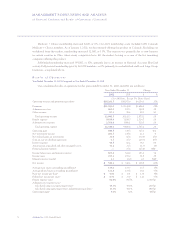
Cost increases for outpatient services were approxi-
mately 12% including the impact of our Trigon acquisi-
tion for the entire rolling 12-month periods, including
periods prior to July 31, 2002. Excluding the impact of
our Trigon acquisition, our outpatient services trend was
approximately one percentage point higher. Drivers of
this outpatient trend include a continuing shift of certain
procedures such as certain cardiac care procedures previ-
ously performed in an inpatient setting to an outpatient
setting and increased cost of emergency room services as
more procedures are being performed at each emergency
room visit. Costs are also increasing for outpatient surgery
and radiology services.
Pharmacy costs increased by approximately 16%
including the impact of our Trigon acquisition for the
entire rolling 12-month periods, including periods prior
to July 31, 2002. Excluding the impact of our Trigon
acquisition, our pharmacy cost trend remained consistent
at approximately 16%. Increases were primarily due to
the introduction of new, higher cost drugs and higher
overall utilization as a result of increases in direct-to-con-
sumer advertising by pharmaceutical companies and
expanded physician-prescribed use of drugs that manage
chronic conditions such as high cholesterol. In response
to increasing pharmacy costs, we are evaluating different
plan designs, recontracting with retail pharmacies and
continuing the implementation of tiered drug benefits for
our members. Three-tier drug programs reflect benefit
designs that have three different co-payment levels,
which depend on the drug selected. Generic drugs have