Anthem Blue Cross 2002 Annual Report Download - page 44
Download and view the complete annual report
Please find page 44 of the 2002 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
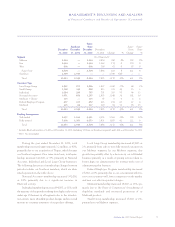
MANAGEMENT’S DISCUSSION AND ANALYSIS
of Financial Condition and Results of Operations (Continued)
Anthem, Inc. 2002 Annual Report 39
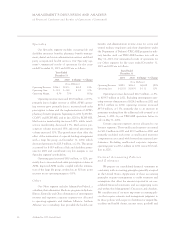
Operating gain increased $17.8 million, or 54%, pri-
marily due to increased mail-order prescription volume
and additional margin resulting from further penetration
of generic drug prescriptions at APM. Improved results in
the life and dental businesses also contributed to the
growth in operating gain, which was modestly offset by
start-up and integration expenses associated with our
behavioral health, vision and dental operations.
Other
Our Other segment includes AdminaStar Federal, a
subsidiary that administers Medicare programs in Indiana,
Illinois, Kentucky and Ohio; elimination of intersegment
revenue and expenses; and corporate expenses not allo-
cated to operating segments. In 2001, our Other segment
also contained Anthem Alliance, a subsidiary that pro-
vided the health care benefits and administration in nine
states for active and retired military employees and their
dependents under the Department of Defense’s TRI-
CARE program for military families. Our TRICARE
operations were sold on May 31, 2001. Our summarized
results of operations for our Other segment for the years
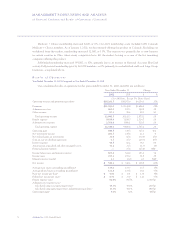
ended December 31, 2002 and 2001 are as follows:
Years Ended
December 31
2002 2001 $ Change % Change
($ in Millions)
Operating
Revenue $(123.9) $189.5 $(313.4) (165)%
Operating Loss $ (91.4) $(23.8) $ (67.6) (284)%
Operating revenue decreased $313.4 million to
$(123.9) million in 2002 from $189.5 million in 2001.
Excluding intersegment operating revenue eliminations of
$302.1 million in 2002 and $214.0 million in 2001, oper-
ating revenue decreased $225.3 million, or 56%, primarily
due to the sale of our TRICARE operations. Excluding our
TRICARE operations from 2001 and intersegment oper-
ating revenue eliminations, operating revenue increased
$37.9 million, or 27%, primarily due to revenue from our
AdminaStar Federal’s 1-800 Medicare Help Line con-
tract. This contract is with CMS for our operation of the
1-800 Medicare Help Line. During the fourth quarter of
2002, CMS awarded this contract to a different company,
despite our superior performance ratings earned each year
since receiving the contract in 1997. We will begin tran-
sitioning this contract to the new contractor beginning
April 1, 2003.
Operating loss increased $67.6 million primarily due
to higher unallocated corporate expenses and the absence
of TRICARE operating gain. These unallocated expenses
accounted for $91.3 million in 2002 and $33.0 million in
2001. This increase in unallocated corporate expenses
was primarily related to higher incentive compensation
costs associated with better than expected operating
results. Also contributing to this increased operating loss
was the reduction in our carrying value of our investment
in MedUnite.
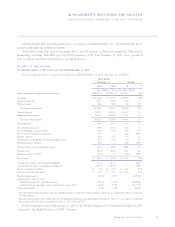
Membership—December 31, 2001
Compared to December 31, 2000
We categorized our membership into eight different
customer types: Local Large Group, Small Group,
Individual, National Accounts, Medicare + Choice,
Federal Employee Program, Medicaid and TRICARE.
The first seven customer types are consistent with those
described in the “Membership—December 31, 2002
Compared to December 31, 2001” discussion. Our TRI-
CARE program provided managed care services to active
and retired military personnel and their dependents. We
sold our TRICARE business on May 31, 2001, and thus
we had no TRICARE members as of December 31, 2001.