Anthem Blue Cross 2002 Annual Report Download - page 52
Download and view the complete annual report
Please find page 52 of the 2002 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
MANAGEMENT’S DISCUSSION AND ANALYSIS
of Financial Condition and Results of Operations (Continued)
Anthem, Inc. 2002 Annual Report 47
other intangible assets, our investment portfolio and
retirement benefits, which are discussed below. Our sig-
nificant accounting policies are also summarized in Note
1 to our audited consolidated financial statements for the
years ended December 31, 2002, 2001 and 2000.
Liability for Unpaid Life, Accident and Health Claims
The most significant accounting estimate in our
consolidated financial statements is our liability for
unpaid life, accident and health claims. This liability was
$1,826.0 million and represented 26% of our total consol-
idated liabilities at December 31, 2002. We record this
liability and the corresponding benefit expense for pend-
ing claims and claims that are incurred but not reported.
Pending claims are those received by us, but not yet
processed through our systems. We determine the amount
of this liability for each of our business segments by fol-
lowing a detailed process that entails using both historical
claim payment patterns as well as emerging medical cost
trends to project our best estimate of claim liabilities. We
also look back to assess how our prior periods’ estimates
developed. To the extent appropriate, changes in such
development are recorded as a change to current period
claims expense. Since the average life of most claims is
just a few months, current medical cost trends and utiliza-
tion patterns are very important in our estimate of claims
liabilities. For information regarding our cost trends, refer
to the discussion of benefit expenses included within this
Management’s Discussion and Analysis.
In addition to the pending claims and incurred but
not reported claims, the liability for unpaid life, accident
and health claims includes reserves for premium deficiency
losses. The premium deficiency losses are recognized
when it is probable that expected claims and loss adjust-
ment expenses will exceed future premiums on existing
health and other insurance contracts without considera-
tion of investment income. For purposes of premium
deficiency losses, contracts are grouped in a manner
consistent with our method of acquiring, servicing and
measuring the profitability of such contracts.
Management constantly reviews its assumptions
regarding our claims liabilities, and makes adjustments to
claims expense recorded, if necessary, in the period it
deems appropriate. If it is determined that management’s
assumptions regarding cost trends and utilization are sig-
nificantly different than actual results, our income state-
ment and financial position could be impacted in future
periods. Adjustments of prior year estimates may result
in additional benefit expense or a reduction of benefit
expense in the period an adjustment is made. Further, due
to the considerable variability of health care costs, adjust-
ments to claims liabilities occur each quarter and are
sometimes significant as compared to the total expense
recorded in that quarter.
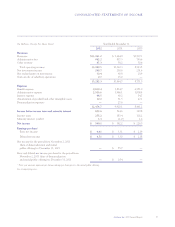
Note 8 to our audited consolidated financial state-
ments for the years ended December 31, 2002, 2001 and
2000 provides historical information regarding the accrual
and payment of our unpaid claims liability. Components
of the total incurred claims for each year include amounts
accrued for current year estimated claims expense as well
as adjustments to prior year estimated accruals.
In Note 8, the line labeled “incurred related to prior
years” accounts for those adjustments made to prior year
estimates. The impact of any reduction of “incurred related
to prior years” claims may be offset as we re-establish the
“incurred related to current year”. Our reserving practice
is to consistently recognize the actuarial best estimate of
our ultimate liability for our claims within a level of con-
fidence required to meet actuarial standards. Thus, only
when the release of a prior year reserve is not offset with
the same level of conservatism in estimating the current
year reserve will the redundancy reduce benefit expense.
When we recognize a release of the redundancy, we dis-
close the amount that is other than our normal release
being experienced. An example of a redundancy release is
discussed in the “Results of Operations—Year Ended
December 31, 2002 and 2001” included elsewhere in this
Management Discussion and Analysis.
We believe we have consistently applied this
methodology in determining our best estimate for unpaid
claims liability each year. This is demonstrated by com-
paring prior year redundancies to total incurred claims
recorded in each past year. This metric was 1.3% in 2000,
1.5% in 2001 and 1.9% at the end of 2002. When this
metric remains constant or increases, it is an indication of
the consistency of our reserving procedures and policies.