Anthem Blue Cross 2002 Annual Report Download - page 66
Download and view the complete annual report
Please find page 66 of the 2002 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
NOTES
to Consolidated Financial Statements (Continued)
Anthem, Inc. 2002 Annual Report 61
years for computer software. Leasehold improvements are
depreciated over the term of the related lease.
Goodwill and Other Intangible Assets: On January 1,
2002, the Company adopted FAS 141, Business Combina-
tions, and FAS 142, Goodwill and Other Intangible Assets.
FAS 141 requires business combinations completed after
June 30, 2001 to be accounted for using the purchase
method of accounting. It also specifies the types of
acquired intangible assets that are required to be recog-
nized and reported separately from goodwill. Under FAS
142, goodwill and other intangible assets with indefinite
lives are not amortized but are tested for impairment at
least annually. Goodwill represents the excess of cost of
acquisition over the fair value of net assets acquired.
Other intangible assets represent the values assigned to
subscriber bases, provider and hospital networks, Blue
Cross and Blue Shield trademarks, licenses, non-compete
and other agreements.
Policy Liabilities: Liabilities for unpaid claims include
estimated provisions for both reported and unreported
claims incurred on an undiscounted basis, as well as esti-
mated provisions for expenses related to the processing of
claims. The liabilities are adjusted regularly based on his-
torical experience and include estimates of trends in
claim severity and frequency and other factors, which
could vary as the claims are ultimately settled. Although
it is not possible to measure the degree of variability
inherent in such estimates, management believes these
liabilities are adequate.
Future policy benefits include liabilities for life insur-
ance future policy benefits of $175.3 and $176.4 at
December 31, 2002 and 2001, respectively, and represent
primarily group term benefits determined using standard
industry mortality tables with interest rates ranging from
2.5% to 6.5%.
Other policyholder liabilities include certain case-
specific reserves as well as rate stabilization reserves asso-
ciated with retrospective rated insurance contracts. Rate
stabilization reserves represent accumulated premiums
that exceed what customers owe based on actual claim
experience and are paid based on contractual requirements.
Premium deficiency losses are recognized when it
is probable that expected claims and loss adjustment
expenses will exceed future premiums on existing health
and other insurance contracts without consideration of
investment income. For purposes of premium deficiency
losses, contracts are deemed to be either short or long
duration and are grouped in a manner consistent with the
Company’s method of acquiring, servicing and measuring
the profitability of such contracts. Once established, pre-
mium deficiency losses are amortized over the remaining
life of the contract.
Retirement Benefits: Retirement benefits represent out-
standing obligations for retiree medical, life, vision and
dental benefits and any unfunded liabilities related to
defined benefit pension plans. Unfunded liabilities for
pension benefits are accrued in accordance with FAS 87,
Employers’ Accounting for Pensions. Benefits for retiree
medical, life, vision and dental benefits are accrued in
accordance with FAS 106, Employers’ Accounting for
Postretirement Benefits Other Than Pensions.
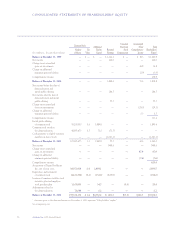
Comprehensive Income: Comprehensive income includes
net income, the change in unrealized gains (losses) on
investments and the change in the additional minimum
pension liability.
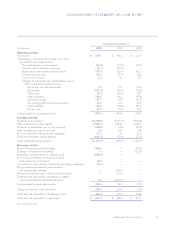
Revenue Recognition: Gross premiums for fully-insured
contracts are recognized as revenue over the period insur-
ance coverage is provided. Premiums applicable to the
unexpired contractual coverage periods are reflected in
the accompanying consolidated balance sheets as unearned
income. Premiums include revenue from retrospective
rated contracts where revenue is based on the estimated
ultimate loss experience of the contract. Premium rev-
enue includes an adjustment for retrospective rated
refunds based on an estimate of incurred claims. Premium
rates for certain lines of business are subject to approval
by the Department of Insurance of each respective state.
Administrative fees include revenue from certain
group contracts that provide for the group to be at risk for
all, or with supplemental insurance arrangements, a por-
tion of their claims experience. The Company charges
these self-funded groups an administrative fee, which is
based on the number of members in a group or the group’s
claim experience. In addition, administrative fees include
amounts received for the administration of Medicare or
certain other government programs. Such fees are based
on a percentage of the claim amounts processed or a com-
bination of a fixed fee per claim plus a percentage of the