Express Scripts 2009 Annual Report Download - page 47
Download and view the complete annual report
Please find page 47 of the 2009 Express Scripts annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
Express Scripts 2009 Annual Report
45
Item 7 – Management’s Discussion and Analysis of Financial Condition and Results of Operations
OVERVIEW
As one of the largest full-service pharmacy benefit management (“PBM”) companies in North America, we
provide health care management and administration services on behalf of our clients, which include health maintenance
organizations, health insurers, third-party administrators, employers, union-sponsored benefit plans, workers’ compensation
plans, and government health programs. During the first quarter of 2009, we changed our reportable segments to
Pharmacy Benefit Management (“PBM”) and Emerging Markets (“EM”). Segment disclosures for 2008 and 2007 have
been reclassified to reflect the new structure. Under the new structure, our integrated PBM services include network claims
processing, home delivery services, patient care and direct specialty home delivery to patients, benefit plan design
consultation, drug utilization review, formulary management, drug data analysis services, distribution of injectable drugs to
patient homes and physicians offices, bio-pharma services, and fulfillment of prescriptions to low-income patients through
manufacturer-sponsored patient assistance programs and company-sponsored generic patient assistance programs.
Through our EM segment, we provide services including distribution of pharmaceuticals and medical supplies to
providers and clinics, distribution of sample units to physicians and verification of practitioner licensure, fertility services to
providers and patients, and healthcare administration and implementation of consumer-directed healthcare solutions.
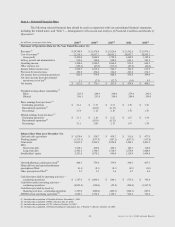
Revenue generated by our segments can be classified as either tangible product revenue or service revenue. We
earn tangible product revenue from the sale of prescription drugs by retail pharmacies in our retail pharmacy networks and
from dispensing prescription drugs from our home delivery and specialty pharmacies. Service revenue includes
administrative fees associated with the administration of retail pharmacy networks contracted by certain clients, medication
counseling services, certain specialty distribution services, and sample fulfillment and accountability services. Tangible
product revenue generated by our PBM and EM segments represented 98.8% of revenues for the year ended December 31,
2009 as compared to 98.7% and 98.6% for the years ended December 31, 2008 and 2007, respectively.
RECENT DEVELOPMENTS
On December 1, 2009, we completed the purchase of the shares and equity interests of certain subsidiaries of
WellPoint that provide pharmacy benefit management services (“NextRx” or the “PBM Business”), in exchange for total
consideration of $4.675 billion paid in cash, which is subject to a purchase price adjustment for working capital. The
NextRx PBM Business is a national provider of PBM services, and we believe the acquisition will enhance our ability to
achieve cost savings, innovations, and operational efficiencies which will benefit our customers and stockholders. The
purchase price was primarily funded through a $2.5 billion underwritten public offering of senior notes completed on June
9, 2009 resulting in net proceeds of $2,478.3 million, and a public offering of 26.45 million shares of common stock
completed June 10, 2009 resulting in net proceeds of $1,569.1 million. Our PBM operating results include those of the
NextRx PBM Business beginning on December 1, 2009, the date of acquisition (see Note 3).
In November 2009, we implemented a new contract with the United States Department of Defense (“DoD”).
While we have provided services to the DoD since 2003, this new contract combines the pharmacy network services, home
delivery and specialty pharmacy under one program. The DoD’s TRICARE Pharmacy Program is the military healthcare
program serving active-duty service members, National Guard and Reserve members and retirees, as well as their
dependents. Under the new contract, we provide online claims adjudication, home delivery services, specialty pharmacy
clinical services, claims processing and contact center support, and other services critical to managing pharmacy trend.
Prior to the new contract, we administered the DoD’s network pharmacy contracts and earned an administrative fee,
therefore related revenues were recorded on a net basis. Due to the expansion of services provided under the new contract,
our method of accounting for revenues and cost of revenues changed to a gross basis. Ingredient cost and member co-
payments are included in revenues and cost of revenues (see Note 1 – Summary of significant accounting policies for a
description of revenue recognition policies).
In the fourth quarter of 2009, construction began on a new state of the art pharmacy fulfillment facility in St.
Louis, Missouri. We expect to take possession of this leased facility during the second quarter of 2010. The new facility
will feature cutting-edge pharmacy automation for the dispensing, packaging and shipment of approximately 110,000
prescriptions per day. We believe this increase in capacity enhances our ability to serve members and allows for future
growth of home delivery services.