CVS 2015 Annual Report Download - page 66
Download and view the complete annual report
Please find page 66 of the 2015 CVS annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
64 CVS Health
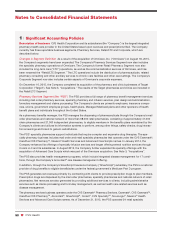
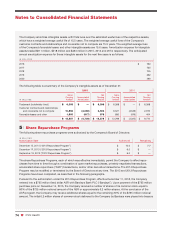
Notes to Consolidated Financial Statements
programs are generally less than billed charges. The Company monitors its revenues and receivables from these
reimbursement sources, as well as other third party insurance payors, and record an estimated contractual allow-
ance for sales and receivable balances at the revenue recognition date, to properly account for anticipated
differences between billed and reimbursed amounts. Accordingly, the total net sales and receivables reported in
the Company’s consolidated financial statements are recorded at the amount expected to be ultimately received
from these payors. Since billing functions for a portion of the Company’s revenue systems are largely computerized,
enabling online adjudication at the time of sale to record net revenues, the Company’s exposure in connection with
estimating contractual allowance adjustments is limited primarily to unbilled and initially rejected Medicare, Medicaid
and third party claims (typically approved for reimbursement once additional information is provided to the payor).
For the remaining portion of the Company’s revenue systems, the contractual allowance is estimated for all billed,
unbilled and initially rejected Medicare, Medicaid and third party claims. The Company evaluates several criteria in
developing the estimated contractual allowances on a monthly basis, including historical trends based on actual
claims paid, current contract and reimbursement terms, and changes in customer base and payor/product mix.
Contractual allowance estimates are adjusted to actual amounts as cash is received and claims are settled, and
the aggregate impact of these resulting adjustments was not significant to our results of operations for any of the
periods presented.
Patient co-payments associated with Medicare Part D, certain state Medicaid programs, Medicare Part B and
certain third party payors are typically not collected at the time products are delivered or services are rendered, but
are billed to the individuals as part of our normal billing procedures and subject to our normal accounts receivable
collections procedures.
Health Care Clinics
For services provided by our health care clinics, revenue recognition occurs for completed
services provided to patients, with adjustments taken for third party payor contractual obligations and patient direct
bill historical collection rates.
Loyalty Program
The Company’s customer loyalty program, ExtraCare®, is comprised of two components,
ExtraSavingsTM and ExtraBucks® Rewards. ExtraSavings coupons redeemed by customers are recorded as a
reduction of revenues when redeemed. ExtraBucks Rewards are accrued as a charge to cost of revenues when
earned, net of estimated breakage. The Company determines breakage based on historical redemption patterns.
See Note 13 for additional information about the revenues of the Company’s business segments.
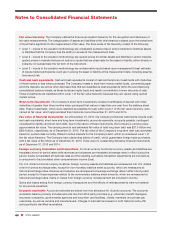
Cost of Revenues
Pharmacy Services Segment
The PSS’ cost of revenues includes: (i) the cost of prescription drugs sold during
the reporting period directly through its mail service dispensing pharmacies and indirectly through its retail pharmacy
network, (ii) shipping and handling costs, and (iii) the operating costs of its mail service dispensing pharmacies and
client service operations and related information technology support costs including depreciation and amortization.
The cost of prescription drugs sold component of cost of revenues includes: (i) the cost of the prescription drugs
purchased from manufacturers or distributors and shipped to members in clients’ benefit plans from the PSS’
mail service dispensing pharmacies, net of any volume-related or other discounts (see “Vendor allowances
and purchase discounts” on the following page) and (ii) the cost of prescription drugs sold (including Retail
Co-Payments) through the PSS’ retail pharmacy network under contracts where it is the principal, net of any
volume-related or other discounts.
Retail/LTC Segment
The RLS’ cost of revenues includes: the cost of merchandise sold during the reporting period
and the related purchasing costs, warehousing and delivery costs (including depreciation and amortization) and
actual and estimated inventory losses.
See Note 13 for additional information about the cost of revenues of the Company’s business segments.