Cigna 2011 Annual Report Download - page 99
Download and view the complete annual report
Please find page 99 of the 2011 Cigna annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
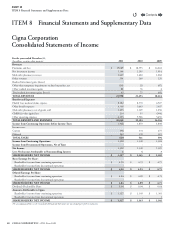
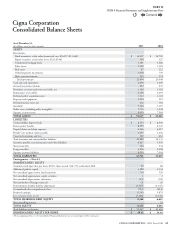
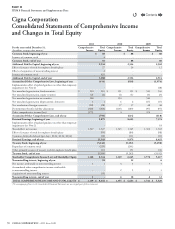
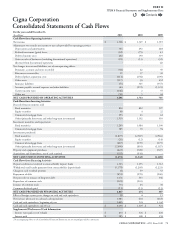
77CIGNA CORPORATION2011 Form10K
PART II
ITEM 8 Financial Statements and Supplementary Data
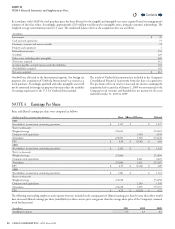
N. Health Care Medical Claims Payable
Medical claims payable for the Health Care segment include both
reported claims and estimates for losses incurred but not yet reported.
e Company develops estimates for Health Care medical claims
payable using actuarial principles and assumptions consistently applied
each reporting period, and recognizes the actuarial best estimate of the
ultimate liability within a level of condence, as required by actuarial
standards of practice, which require that the liabilities be adequate
under moderately adverse conditions.
e liability is primarily calculated using “completion factors” (a measure
of the time to process claims), which are developed by comparing the
date claims were incurred, generally the date services were provided,
to the date claims were paid. e Company uses historical completion
factors combined with an analysis of current trends and operational
factors to develop current estimates of completion factors. e Company
estimates the liability for claims incurred in each month by applying
the current estimates of completion factors to the current paid claims
data. is approach implicitly assumes that historical completion rates
will be a useful indicator for the current period. It is possible that the
actual completion rates for the current period will develop dierently
from historical patterns, which could have a material impact on the
Company’s medical claims payable and shareholders’ net income.
Completion factors are impacted by several key items including changes
in: 1) electronic (auto-adjudication) versus manual claim processing,
2) provider claims submission rates, 3) membership and 4) the mix of
products. As noted, the Company uses historical completion factors
combined with an analysis of current trends and operational factors
to develop current estimates of completion factors.
In addition, for the more recent months, the Company also relies on
medical cost trend analysis, which reects expected claim payment
patterns and other relevant operational considerations. Medical cost
trend is primarily impacted by medical service utilization and unit costs,
which are aected by changes in the level and mix of medical benets
oered, including inpatient, outpatient and pharmacy, the impact of
copays and deductibles, changes in provider practices and changes in
consumer demographics and consumption behavior.
Despite reecting both historical and emerging trends in setting reserves,
it is possible that the actual medical trend for the current period will
develop dierently from expectations, which could have a material
impact on the Company’s medical claims payable and shareholders’
net income.
For each reporting period, the Company evaluates key assumptions
by comparing the assumptions used in establishing the medical claims
payable to actual experience. When actual experience diers from the
assumptions used in establishing the liability, medical claims payable are
increased or decreased through current period shareholders’ net income.
Additionally, the Company evaluates expected future developments and
emerging trends which may impact key assumptions. e estimation
process involves considerable judgment, reecting the variability inherent
in forecasting future claim payments. ese estimates are highly sensitive
to changes in the Company’s key assumptions, specically completion
factors, and medical cost trends.
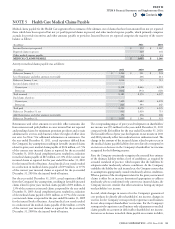
O. Unearned Premiums and Fees
Premiums for life, accident and health insurance are recognized as
revenue on a pro rata basis over the contract period. Fees for mortality
and contract administration of universal life products are recognized
ratably over the coverage period. e unrecognized portion of these
amounts received is recorded as unearned premiums and fees.
P. Accounts Payable, Accrued Expenses
and Other Liabilities
Accounts payable, accrued expenses and other liabilities consist principally
of liabilities for pension, other postretirement and postemployment
benets (see Note9), self-insured exposures, management compensation
and various insurance-related items, including experience rated refunds,
the minimum medical loss ratio rebate accrual under Health Care
Reform, amounts related to reinsurance contracts and insurance-related
assessments that management can reasonably estimate. Accounts payable,
accrued expenses and other liabilities also include certain overdraft
positions and the loss position of certain derivatives, primarily for GMIB
contracts (see Note12). Legal costs to defend the Company’s litigation
and arbitration matters are expensed when incurred in cases that the
Company cannot reasonably estimate the ultimate cost to defend. In
cases that the Company can reasonably estimate the cost to defend,
these costs are recognized when the claim is reported.
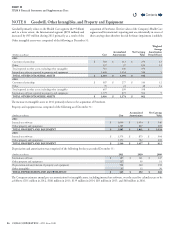
Q. Translation of Foreign Currencies
e Company generally conducts its international business through foreign
operating entities that maintain assets and liabilities in local currencies,
which are generally their functional currencies. e Company uses
exchange rates as of the balance sheet date to translate assets and liabilities
into U.S. dollars. Translation gains or losses on functional currencies, net
of applicable taxes, are recorded in accumulated other comprehensive
income (loss). e Company uses average monthly exchange rates during
the year to translate revenues and expenses into U.S. dollars.
R. Premiums and Fees, Revenues
and Related Expenses
Premiums for group life, accident and health insurance and managed
care coverages are recognized as revenue on a pro rata basis over the
contract period. Benets and expenses are recognized when incurred.
Premiums and fees include revenue from experience-rated contracts
that is based on the estimated ultimate claim, and in some cases,
administrative cost experience of the contract. For these contracts,
premium revenue includes an adjustment for experience-rated refunds
which is calculated according to contract terms and using the customer’s
experience (including estimates of incurred but not reported claims).
Beginning in 2011, premium revenue also includes an adjustment
to reect the estimated eect of rebates due to customers under the
minimum medical loss ratio provisions of Health Care Reform.
Premiums for individual life, accident and health insurance and annuity
products, excluding universal life and investment-related products, are
recognized as revenue when due. Benets and expenses are matched
with premiums.
Contents
Q