Anthem Blue Cross 2001 Annual Report Download - page 34
Download and view the complete annual report
Please find page 34 of the 2001 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
Operating revenue increased $485.0 million, or 12%, in 2000 primarily due to premium rate increases in
group (both Local Large Group and Small Group) and Medicare + Choice businesses, and the effect of
higher average membership throughout the year. Medicare + Choice premium rates increased due to both
the aging of our insured Medicare + Choice population in 2000 and a 3% rate increase from CMS at the
beginning of 2000. We receive higher premiums from CMS as our Medicare + Choice population ages.
Medicare + Choice membership increased 28% due to reduced competition in the Ohio marketplace as a
result of competitors discontinuing their participation in the Medicare + Choice product.
Operating gain increased $51.4 million, or 141%, resulting in an operating margin of 2.0%, a 110 basis
point improvement from the year ended December 31, 1999. Operating gain increased primarily due to our
growth in premiums and improved underwriting results.
Membership increased 5% to 4.6 million members, primarily due to growth in our National, BlueCard and
Local Large Group businesses.
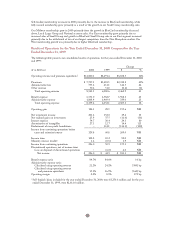
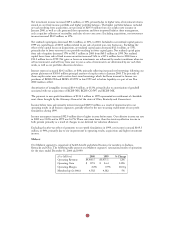
East
Our East segment is comprised of health benefit and related business for members in Connecticut, New
Hampshire and Maine. The following table presents our East segment’s summarized results of operations
for the years ended December 31, 2000 and 1999. BCBS-NH is included from its October 27, 1999,
acquisition date and BCBS-ME is included from its acquisition date of June 5, 2000.
($ in Millions) 2000 1999 % Change
Operating Revenue $2,921.9 $1,598.9 83%0
Operating Gain (Loss) $ 103.8 $ (0.9) NM0
Operating Margin 3.6% (0.1)% 370 bp
Membership (in 000s) 2,093 1,397 50%0
Operating revenue increased $1,323.0 million, or 83%, primarily due to an increase in premiums, resulting
from our acquisitions of BCBS-NH in October 1999 and BCBS-ME in June 2000 and the conversion of
the State of Connecticut account from self-funded to fully insured status in July 1999. Due to the State of
Connecticut’s conversion, 2000 included a full year of premiums versus six months of premiums (July
through December) in 1999. For the first six months of 1999, we recorded administrative fee income for
the State of Connecticut account. Excluding the effect of acquisitions and the conversion of the State of
Connecticut account, premiums increased $155.7 million, or 12%, in 2000 due to premium rate increases in
our group business and higher average membership.
Operating gain increased $104.7 million and our operating margin increased 370 basis points as the effect
of disciplined pricing, expense control and membership growth all contributed to the improvement in
operating earnings. Additionally, administrative expense in 1999 included $41.9 million resulting from our
settlement with the OIG, Health and Human Services to resolve an investigation into alleged misconduct
in the Medicare fiscal intermediary operations in Connecticut during periods preceding BCBS-CT’s merger
with Anthem.
Membership increased 50% to 2.1 million in 2000 primarily due to our acquisition of BCBS-ME and
growth in both our Local Large Group and Small Group and our National businesses. Excluding our
acquisition of BCBS-ME, membership grew 15%.
32