Anthem Blue Cross 2001 Annual Report Download - page 13
Download and view the complete annual report
Please find page 13 of the 2001 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.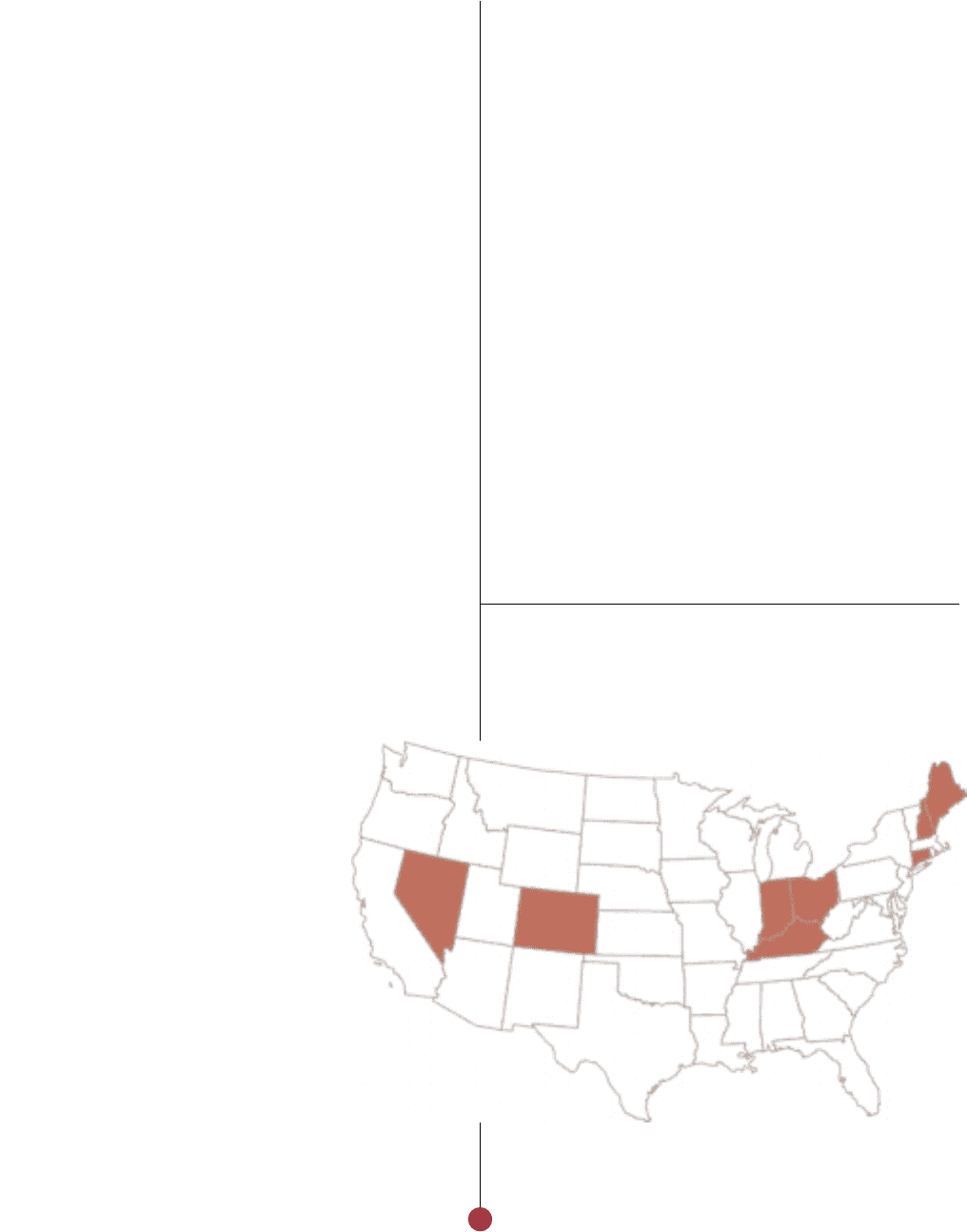
Asthma Initiative project. In Colorado and Nevada,
we recently began partnering with physicians to help
them intensively manage the health of members with
one of 14 rare or complex diseases, including cystic
fibrosis, systemic lupus and multiple sclerosis. Anthem
has successfully collaborated with more than 300
hospitals in the Midwest on a nationally recognized
quality program designed to help them better use
clinical data, monitoring, outcomes and best practices
to improve care and promote patient safety. These are
just a few examples of local and regional programs
that we expect will produce solid health improvement
results for our members.
With health care costs increasing at double-digit levels
in 2001, Anthem focused on measures to carefully
manage and optimize the cost of quality health care
for our members. We were pleased to be able to
reduce slightly Anthem’s consolidated benefit expense
ratio in 2001 compared to 2000, despite continued
increases in the cost of care. While managing very
broad provider networks – usually the broadest
networks in our markets – we were able to maintain
very favorable contract arrangements. In addition, our
integrated pharmacy benefit management company,
Anthem Prescription Management, helped us manage
our drug expenses.
We continued to develop innovative, effective
disease management initiatives to optimize the cost
of care while helping members better manage
chronic health conditions. Disease management
programs – developed in conjunction with physicians
and other health care professionals – seek to address
chronic conditions before they require
extensive treatments, costly trips to the
emergency room or hospitalization.
Through these initiatives, clinical quality
and outcomes for certain conditions can
be greatly improved.
In Maine, our asthma program
was named one of the top two asthma disease
management programs in the country by the Tufts
University School of Medicine’s Asthma Care and
Taking Great Strides:
Optimizing the cost of health care
11
Anthem, which is based in Indianapolis, Indiana,
is the exclusive Blue Cross and Blue Shield licensee
in Indiana, Kentucky, Ohio, Connecticut, New
Hampshire, Maine, Colorado and Nevada.