Anthem Blue Cross 2001 Annual Report Download - page 20
Download and view the complete annual report
Please find page 20 of the 2001 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
Management’s Discussion and Analysis of Financial Condition
and Results of Operations
Introduction
We are one of the nation’s largest health benefits companies and an independent licensee of the Blue Cross
Blue Shield Association, or BCBSA. We offer Blue Cross Blue Shield branded products to nearly eight
million members throughout Indiana, Kentucky, Ohio, Connecticut, New Hampshire, Maine, Colorado
and Nevada.
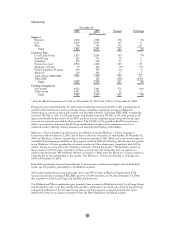
Our reportable segments are strategic business units delineated by geographic areas within which we offer
similar products and services. We manage our business units with a local focus to address each geographic
region’s unique market, regulatory and healthcare delivery characteristics. Our segments are: Midwest, which
includes Indiana, Kentucky and Ohio; East, which includes Connecticut, New Hampshire and Maine; and
West, which includes Colorado and Nevada.
In addition to our three geographic segments, we operate a Specialty segment that includes business units
providing group life and disability insurance benefits, pharmacy benefit management, dental and vision
administration services and third party occupational health services. Our Other segment is comprised of
AdminaStar Federal, Anthem Alliance Health Insurance Company, or Anthem Alliance, intersegment
revenue and expense eliminations and corporate expenses not allocated to reportable segments. AdminaStar
Federal is a subsidiary that administers Medicare programs in Indiana, Illinois, Kentucky and Ohio.
Anthem Alliance is a subsidiary that primarily provided health care benefits and administration in nine
states for the Department of Defense’s TRICARE Program for military families until we sold our
TRICARE operations on May 31, 2001.
We offer traditional indemnity products and a diversified mix of managed care products, including health
maintenance organizations or HMOs, preferred provider organizations or PPOs, and point of service or
POS plans. We also provide a broad array of managed care services and partially insured products to self-
funded employers, including underwriting, stop loss insurance, actuarial services, provider network access,
medical cost management, claims processing and other administrative services. Our operating revenue
consists of premiums, benefit plan administrative fees and other revenue. The premiums come from fully
insured contracts where we indemnify our policyholders against loss. The administrative fees come from
self-funded contracts where our contract holders are wholly or partially self-insured and from the
administration of Medicare programs. Other revenue is principally generated by our pharmacy benefit
management company in the form of co-pays and deductibles associated with the sale of mail order drugs.
Our benefit expense consists mostly of four cost of care components: outpatient and inpatient care costs,
physician costs and pharmacy benefit costs. All four components are affected both by unit costs and
utilization rates. Unit costs, for example, are the cost of outpatient medical procedures, inpatient hospital
stays, physician fees for office visits and prescription drug prices. Utilization rates represent the volume of
consumption of health services and vary with the age and health of our members and broader social and
lifestyle factors in the population as a whole.
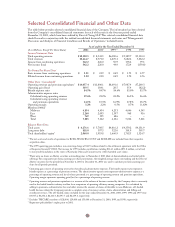
Our results in 1999, 2000 and 2001 were significantly impacted by the acquisitions of Blue Cross and Blue
Shield of New Hampshire, or BCBS-NH, which we completed on October 27, 1999, Blue Cross and Blue
Shield of Colorado and Nevada, or BCBS-CO/NV, which we completed on November 16, 1999, and Blue
Cross and Blue Shield of Maine, or BCBS-ME, which we completed on June 5, 2000. We accounted for
these acquisitions as purchases and we included the net assets and results of operations in our consolidated
financial statements from the respective dates of purchase. The following represents the contribution to our
total revenues, operating gain, assets and membership in the year of and subsequent to each acquisition for
the years ended December 31, 2001, 2000 and 1999.
18