Anthem Blue Cross 2001 Annual Report Download - page 22
Download and view the complete annual report
Please find page 22 of the 2001 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
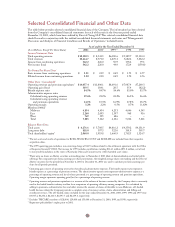
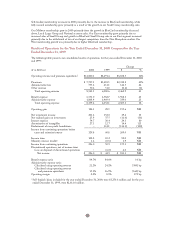
Membership – Year Ended December 31, 2001 Compared to Year Ended
December 31, 2000
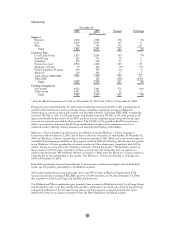
We categorize our membership into eight different customer types: Local Large Group, Small Group,
Individual, National, Medicare + Choice, Federal Employee Program, Medicaid and TRICARE.
• Local Large Group consists of those customers with 51 or more eligible employees, which are not
considered National accounts.
• Small Group consists of those customers with one to 50 employees.
• Individual members include those in our under age 65 business and our Medicare Supplement
(age 65 and over) business.
• Our National accounts customers are employer groups, which have multi-state locations and require
partnering with other Blue Cross and Blue Shield plans for administration and/or access to non-
Anthem provider networks. Included within the National business are our BlueCard customers who
represent enrollees of health plans marketed by other Blue Cross and Blue Shield Plans, or the home
plans, who receive health care services in our Blue Cross and Blue Shield licensed markets.
• Medicare + Choice members have enrolled in coverages that are managed care alternatives for the
Medicare program.
• The Federal Employee Program, or FEP, provides health insurance coverage to United States
government employees and their dependents. Our FEP members work in Anthem markets and are
covered by this program.
• Medicaid membership represents eligible members with state sponsored managed care alternatives in
the Medicaid program which we manage for the states of Connecticut and New Hampshire.
• Our TRICARE program provided managed care services to active and retired military personnel and
their dependents. We sold our TRICARE business on May 31, 2001, and thus we had no TRICARE
members as of December 31, 2001. At December 31, 2000, our TRICARE membership totaled
128,000, was fully insured and included in the Midwest segment.
Our BlueCard membership is calculated based on the amount of BlueCard administrative fees we receive
from the BlueCard members’ home plans. Generally, the administrative fees we receive are based on the
number and type of claims processed and a portion of the network discount on those claims. The
administrative fees are then divided by an assumed per member per month, or PMPM, factor to calculate
the number of members. The assumed PMPM factor is based on an estimate of our experience and
BCBSA guidelines.
In addition to categorizing our membership by customer type, we categorize membership by funding
arrangement according to the level of risk we assume in the product contract. Our two funding arrangement
categories are fully insured and self-funded. Self-funded products are offered to customers, generally larger
employers, with the ability and desire to retain some or all of the risk associated with their employees’ health
care costs.
The renewal patterns of our membership are somewhat cyclical throughout the year. Typically,
approximately 37% of our group fully insured business renews during the first quarter and approximately
30% renews during the third quarter. The remainder of our membership renewals are evenly distributed
over the other two quarters.
The following table presents our membership count by segment, customer type and funding arrangement as
of December 31, 2001 and 2000. The membership data presented are unaudited and in certain instances
include our estimates of the number of members represented by each contract at the end of the period,
rounded to the nearest thousand.
20