Anthem Blue Cross 2001 Annual Report Download
Download and view the complete annual report
Please find the complete 2001 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
Taking Great Strides
2001 Annual Report
Table of contents
-
Page 1
2001 Annual Report Taking Great Strides -
Page 2
... the Cost of Health Care ...11 Developing Our Associates ...12 Improving the Level of Service to Our Customers ...12 CAQH: Making Health Care Easier and Better for Consumers and Physicians ...13 Improving the Health of Our Members...14 Improving the Health of Our Communities ...15 Financial Review... -
Page 3
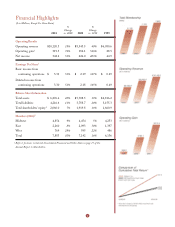
Financial Highlights ($ in Millions, Except Per Share Data) 2001 % Change vs. 2000 2000 % Change vs. 1999 1999 Operating Results Operating revenue Operating gain1 Net income Earnings Per Share 1 $10,120.3 319.5 342.2 18% 74% 51% $ 8,543.5 184.1 226.0 40% 546% 403% $ 6,080.6 28.5 44.9 ... -
Page 4
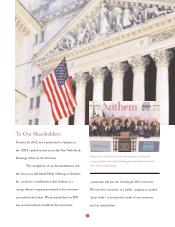
... in history. We view the conversion to a public company as another "great stride" as we meet the needs of our customers and our shareholders. Anthem, Inc. board members and leadership team celebrate the closing of Anthem's ï¬rst day of trading from the bell podium at the New York Stock Exchange. 2 -
Page 5
...most respected brand in health care. This was evident in the growth of our national account business, which beneï¬ted from the unique advantages of the Blue Cross and Blue Shield Association's BlueCard program. We already hold a leading market position in seven of our eight states, yet we continue... -
Page 6
... Cross and Blue Shield of Kansas. Although that proposed transaction was approved credit facilities to provide appropriate liquidity to fund our future operations. Our overall performance is an outcome of providing the products our customers need and value. Health care quality and customer service... -
Page 7
... associations working to improve care, keep health care affordable and simplify administration and processes for customers and physicians. We addressed a sometimes-chaotic legislative and regulatory environment at the national and state levels. Congress and state legislatures debated proposed new... -
Page 8
... are: • • • Diversity in products, geography and customer mix; Afï¬liation with the Blue Cross and Blue Shield brand; Discipline in underwriting, medical cost management, expense control and integration of operations; Key members of our senior management team are, from left to right (front... -
Page 9
... In 2001, Anthem experienced growth, as our membership climbed to 7.9 million members; change, as we successfully completed our demutualization and became a publicly traded company; and success, as we continued to work toward our goal of becoming one of the nation's largest and best health bene... -
Page 10
... membership reached 7.9 million, an increase of 10 percent over 2000 on a same-store basis. This makes Anthem Blue Cross Blue Shield national network of health care providers and allows members to receive care and customer service when they travel or are living outside their home plan's service area... -
Page 11
... groups that have the option of selecting a pharmacy beneï¬t manager, and is now providing service to customers in all eight Anthem states. • Our dental beneï¬ts company began building provider networks in the Anthem East states and converted nearly 500,000 members in Anthem Midwest to a new... -
Page 12
... Week magazine's annual survey of the nation's largest, most innovative organizations. Information Week also presented Anthem with medals in business practices, technology, eBusiness strategies and customer knowledge. As we continue to consolidate our operating systems and improve our processes... -
Page 13
... disease management programs in the country by the Tufts University School of Medicine's Asthma Care and Anthem, which is based in Indianapolis, Indiana, is the exclusive Blue Cross and Blue Shield licensee in Indiana, Kentucky, Ohio, Connecticut, New Hampshire, Maine, Colorado and Nevada. Asthma... -
Page 14
... associates, yielded signiï¬cantly improved results in service both to our customers and to the health care professionals who comprise our networks. We remain on track to reduce our number of core operating systems by the end of 2003. During 2001, Anthem's overall customer retention rate exceeded... -
Page 15
...cer of the coalition. Many Anthem associates worked in company-wide teams to implement internal changes to meet or exceed CAQH guidelines, and Anthem Blue Cross and Blue Shield health plans participated in several signiï¬cant CAQH programs. • Anthem Prescription Management was one of the ï¬rst... -
Page 16
... care programs. Our plans in Connecticut, New Hampshire and Maine achieved "Best in Class" or "Top Performer" designation in two or more preventive care measurements. • Anthem Midwest, our plans in Indiana, Ohio and Kentucky, once again earned the HERA award from the National Managed Health Care... -
Page 17
... Maine Coalition for Safe Kids and New Hampshire Public Television's Speaking of Women's Health conference. Our community efforts in Connecticut earned Anthem Blue Cross and Blue Shield the "Corporate Citizen of the Year" award from Business New Haven magazine. In Indiana and Kentucky, Anthem Blue... -
Page 18
... Great Strides: Financial Review Contents Selected Consolidated Financial and Other Data...17 Management's Discussion and Analysis of Financial Condition and Results of Operations ...18 Consolidated Balance Sheets ...41 Consolidated Statements of Income...42 Consolidated Statements of Shareholders... -
Page 19
... and other revenue the amount of claims attributable to non-Medicare, self-funded health business where the Company provides a complete array of customer service, claims administration and billing and enrollment services. The self-funded claims included for the years ended December 31, 2001, 2000... -
Page 20
... a Specialty segment that includes business units providing group life and disability insurance benefits, pharmacy benefit management, dental and vision administration services and third party occupational health services. Our Other segment is comprised of AdminaStar Federal, Anthem Alliance Health... -
Page 21
..., 2001, we signed a definitive agreement with Blue Cross and Blue Shield of Kansas, or BCBS-KS, pursuant to which BCBS-KS would become a wholly owned subsidiary. Under the proposed transaction, BCBS-KS would demutualize and convert to a stock insurance company. The agreement calls for us to pay $190... -
Page 22
... care services in our Blue Cross and Blue Shield licensed markets. • Medicare + Choice members have enrolled in coverages that are managed care alternatives for the Medicare program. • The Federal Employee Program, or FEP, provides health insurance coverage to United States government employees... -
Page 23
... (In Thousands) Segment Midwest East West Total Customer Type Local Large Group Small Group Individual National accounts1 Medicare + Choice Federal Employee Program Medicaid Total without TRICARE TRICARE Total Funding Arrangement Self-funded Fully insured Total 1 Change 272 167 174 613 193 38 51... -
Page 24
... administrative fees and other revenue the amount of claims attributable to non-Medicare, self-funded health business where we provide a complete array of customer service, claims administration and billing and enrollment services. The self-funded claims included for the year ended December 31, 2001... -
Page 25
... BCBS-ME and the sale of our TRICARE business, other revenue, which is comprised principally of co-pays and deductibles associated with Anthem Prescription Management's, or APM's, sale of mail order drugs, increased $12.1 million, or 27%. APM is our pharmacy benefit manager and provides its services... -
Page 26
... in their contracting with health insurance companies as a result of reduced hospital reimbursements from Medicare and pressure to recover the costs of additional investments in new medical technology and facilities. Administrative expense increased $177.7 million, or 10%, in 2001, which includes... -
Page 27
... 4,4541 % Change 14%0 84%0 120 bp 9%0 Excludes 128,000 TRICARE members Operating revenue increased $632.5 million, or 14%, in 2001 due primarily to premium rate increases and the effect of higher average membership in our Local Large Group, Small Group and Medicare + Choice businesses. Operating... -
Page 28
...595 % Change 24%0 704%0 220 bp 29%0 Operating revenue increased $152.0 million, or 24%, primarily due to higher premium rates designed to bring our pricing in line with cost of care and higher membership in National and both Local Large Group and Small Group businesses. Operating gain increased $17... -
Page 29
... business units such as AdminaStar Federal, a subsidiary that administers Medicare Parts A and B programs in Indiana, Illinois, Kentucky and Ohio, and Anthem Alliance, a subsidiary that provided the health care benefits and administration in nine states for active and retired military employees... -
Page 30
Membership Total 2000 Segment Midwest East West Total Customer Type Local Large Group Small Group Individual National accounts1 Medicare + Choice Federal Employee Program Medicaid Total without TRICARE TRICARE Total Funding Type Fully insured Self-funded Total 1 BCBS-ME Acquisition -- 487 -- 487 ... -
Page 31
... above, Local Large Group and National accounts sales. Our East membership grew primarily due to increased sales of Small Group and growth in BlueCard. Small Group sales in our East segment increased primarily due to the withdrawal of two of our largest competitors from the New Hampshire market. Our... -
Page 32
... and Small Group) and higher membership in Medicare + Choice. East premiums increased primarily due to premium rate increases and higher membership in group business, as well as the conversion of the State of Connecticut account to fully insured from self-funded status in mid-1999. Administrative... -
Page 33
... of BCBS-NH, BCBS-CO/NV and BCBS-ME. The payment to non-profit foundations of $114.1 million in 1999 represented our settlement of charitable asset claims brought by the Attorneys General of the states of Ohio, Kentucky and Connecticut. Income before taxes and minority interest increased $269... -
Page 34
... underwriting results. Membership increased 5% to 4.6 million members, primarily due to growth in our National, BlueCard and Local Large Group businesses. East Our East segment is comprised of health benefit and related business for members in Connecticut, New Hampshire and Maine. The following... -
Page 35
... of business, which was the result of improved customer service and a more comprehensive product portfolio. Specialty Our Specialty segment includes our group life and disability, pharmacy benefit management, dental and vision administration services and third party occupational health services... -
Page 36
... business units such as AdminaStar Federal, a subsidiary that administers Medicare Parts A and B programs in Indiana, Illinois, Kentucky and Ohio, and Anthem Alliance, a subsidiary that provided the health care benefits and administration in nine states for active and retired military employees... -
Page 37
... of preserving our asset base. Cash inflows could be adversely impacted by general business conditions including health care costs increasing more than premium rates, our ability to maintain favorable provider agreements, reduction in enrollment, changes in federal and state regulation, litigation... -
Page 38
... debenture. The number of shares to be purchased will be determined based on the average trading price of Anthem common stock at the time of settlement. In addition, we will make quarterly contract fee payments on the purchase contracts at the annual rate of 0.05% of the stated amount of $50... -
Page 39
...1999 included the following non-recurring disbursements of $156.0 million: payments for the settlement of charitable asset claims in the states of Ohio, Kentucky and Connecticut and the settlement with the OIG, Health and Human Services, with respect to BCBS-CT. Net cash used in investing activities... -
Page 40
... Anthem Insurance currently has a $300.0 million commercial paper program available for general corporate purposes. Commercial paper notes are short term senior unsecured notes, with a maturity not to exceed 270 days from date of issuance. When issued, the notes bear interest at current market rates... -
Page 41
...rates and changes in equity market valuations. Potential impacts discussed below are based upon sensitivity analyses performed on Anthem's financial positions as of December 31, 2001. Actual results could vary significantly from these estimates. Our primary objective is the preservation of the asset... -
Page 42
... pricing below market trends of increasing costs; increased government regulation of health benefits and managed care; significant acquisitions or divestitures by major competitors; introduction and utilization of new prescription drugs and technology; a downgrade in our financial strength ratings... -
Page 43
Anthem, Inc. Consolidated Balance Sheets December 31 (In Millions, Except Share Data) Assets Current assets: Investments available-for-sale, at fair value: Fixed maturity securities Equity securities Cash and cash equivalents Premium and self funded receivables Reinsurance receivables Other ... -
Page 44
..., Inc. Consolidated Statements of Income Year ended December 31 (In Millions, Except Per Share Data) Revenues Premiums Administrative fees Other revenue Total operating revenue Net investment income Net realized gains on investments Gain on sale of subsidiary operations 2001 2000 1999 $ 9,244... -
Page 45
Anthem, Inc. Consolidated Statements of Shareholders' Equity Common Stock Number of Par Shares Value Additional Paid in Capital Retained Earnings Accumulated Other Comprehensive Income Total Shareholders' Equity1 (In Millions, Except Share Data) Balance at December 31, 1998 Net income Change in ... -
Page 46
... Proceeds from long term borrowings Payments on long term borrowings Net proceeds from common stock issued in the initial public offering Net proceeds from issuance of Equity Security Units Payments to eligible statutory members in the demutualization Cash provided by financing activities Change in... -
Page 47
... its subsidiary insurance companies are licensed in all states and are Blue Cross Blue Shield Association licensees in Indiana, Kentucky, Ohio, Connecticut, Maine, New Hampshire, Colorado and Nevada. Products include health and group life insurance, managed health care, and government health program... -
Page 48
...is reviewed once the policy period is completed and adjustments are recorded when determined. Premium rates for certain lines of business are subject to approval by the Department of Insurance of each respective state. Administrative fees include revenue from certain group contracts that provide for... -
Page 49
...(see Note 6). The number of shares to be purchased will be determined based on the average trading price of Anthem common stock at the time of settlement. In addition, Anthem will pay quarterly contract fee payments on the purchase contracts at the annual rate of 0.05% of the stated amount of $50.00... -
Page 50
...completed its purchase of substantially all of the assets and liabilities of Associated Hospital Service of Maine, formerly d/b/a Blue Cross and Blue Shield of Maine ("BCBS-ME"), in accordance with the Asset Purchase Agreement dated July 13, 1999. The purchase price was $95.4 (including direct costs... -
Page 51
... benefit of charitable foundations in Kentucky, Ohio, and Connecticut, respectively, from Anthem Insurance's subsidiaries, Anthem Health Plans of Kentucky, Inc., Community Insurance Company and Anthem Health Plans, Inc., respectively. 5. Investments The following is a summary of available-for-sale... -
Page 52
... only with the prior approval of the Indiana Department of Insurance ("DOI"), and only out of capital and surplus funds of Anthem Insurance that the DOI determines to be available for the payment under Indiana insurance laws. For statutory accounting purposes, the surplus notes are considered a part... -
Page 53
... above, Anthem Insurance currently has a $300.0 commercial paper program available for general corporate purposes. Commercial paper notes are short term senior unsecured notes, with a maturity not to exceed 270 days from date of issuance. When issued, the notes bear interest at current market rates... -
Page 54
9. Unpaid Life, Accident and Health Claims The following table provides a reconciliation of the beginning and ending balances for unpaid life, accident and health claims: 2001 Balances at January 1, net of reinsurance Business purchases (divestitures) Incurred related to: Current year Prior years ... -
Page 55
... The Company's 2001 Stock Incentive Plan (the "Stock Plan") provides for the granting of stock options, restricted stock awards, performance stock awards, performance awards and stock appreciation rights to eligible employees and non-employee directors. The Company has registered 7,000,000 shares of... -
Page 56
... including the expected stock price volatility. Because the Company's stock option grants have characteristics significantly different from those of traded options, and because changes in the subjective input assumptions can materially affect the fair value estimate, in management's opinion, the... -
Page 57
... Deferred tax asset (liability) - noncurrent Net deferred tax asset (liability) Significant components of the provision for income taxes consist of the following: 2001 Current tax expense (benefit): Federal State and local Total current tax expense (benefit) Deferred tax expense Total income tax... -
Page 58
...amount computed at the statutory rate is as follows: 2001 Amount Amount at statutory rate State and local income taxes (benefit) net of federal tax benefit Amortization of goodwill Dividends received deduction Deferred tax valuation allowance change, net of net operating loss carryforwards and other... -
Page 59
... Benefits Anthem Insurance and its subsidiary, Anthem Health Plans of New Hampshire, Inc. (which acquired the business of BCBS-NH), sponsor defined benefit pension plans. These plans generally cover all full-time employees who have completed one year of continuous service and attained the age... -
Page 60
...00% 4.50% 9.00% Other Benefits 2001 2000 7.25% 7.50% 4.50% 6.50% 4.50% 6.27% 1999 7.50% 4.50% 6.50% Discount rate Rate of compensation increase Expected rate of return on plan assets The assumed health care cost trend rate used in measuring the other benefit obligations is generally 6% in 2000 and... -
Page 61
... of action under federal and state law. These lawsuits typically allege that the defendant managed care organizations employ policies and procedures for providing health care benefits that are inconsistent with the terms of the coverage documents and other information provided to their members, and... -
Page 62
... Department of Health and Human Services, in the amount of $41.9, to resolve an investigation into misconduct in the Medicare fiscal intermediary operations of Blue Cross & Blue Shield of Connecticut ("BCBS-CT"), AHP's predecessor. The period investigated was before Anthem Insurance merged with BCBS... -
Page 63
... these reviews would not have a material adverse effect on the consolidated financial condition of the Company. As a Blue Cross Blue Shield Association licensee, the Company participates in the Federal Employee Program ("FEP"), a nationwide contract with the Federal Office of Personnel Management to... -
Page 64
...participation in the Federal Employee Program, Medicare, Medicare at Risk, and TRICARE Program, the Company generated approximately 20%, 22% and 23% of its total consolidated revenues from agencies of the U.S. government for the years ended December 31, 2001, 2000 and 1999, respectively. The Company... -
Page 65
... ("Codification") which became effective January 1, 2001. Codification resulted in changes to certain accounting practices that Anthem Insurance and its insurance subsidiaries use to prepare statutory-basis financial statements. The impact of these changes was not significant. $319.5 238.6 60.8 25... -
Page 66
...worth of shares, subject to business and market conditions. Shares may be repurchased in the open market and in negotiated transactions for a period of twelve months beginning February 6, 2002. On May 30, 2001, Anthem Insurance and Blue Cross and Blue Shield of Kansas ("BCBS-KS") signed a definitive... -
Page 67
... protection of assets. At Anthem, we maintain an internal auditing program designed to monitor compliance with policies and procedures and to evaluate the internal control structure. The consolidated financial statements included in this Annual Report have been audited by the Company's independent... -
Page 68
... Ben Lytle Chairman of the Board Anthem, Inc. Susan B. Bayh Distinguished Visiting Professor College of Business Administration Butler University Larry C. Glasscock President and Chief Executive Ofï¬cer Anthem, Inc. William B. Hart Chairman National Trust for Historic Preservation Allan B. Hubbard... -
Page 69
...Dorr President Anthem Blue Cross and Blue Shield Midwest Region Keith R. Faller President Anthem Blue Cross and Blue Shield West Region Caroline S. Matthews Chief Operating Ofï¬cer Anthem Blue Cross and Blue Shield National Accounts Michael D. Houk President Anthem Specialty Business John M. Murphy... -
Page 70
... Circle, Indianapolis, Indiana. Market Price of Common Stock Anthem, Inc.'s common stock began trading on the New York Stock Exchange on October 30, 2001. The following table shows high and low sales prices for the company's common stock as reported on the New York Stock Exchange Composite Tape for... -
Page 71
-
Page 72
120 Monument Circle Indianapolis, Indiana 46204 wwww.anthem.com 2320-AR-0402