Quest Diagnostics 2003 Annual Report Download - page 55
Download and view the complete annual report
Please find page 55 of the 2003 Quest Diagnostics annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.total cost to comply with Medicare administrative requirements is disproportionate to our cost to bill other
payers, average Medicare reimbursement rates approximate the Company’s overall average reimbursement rate
from all payers, making this business generally less profitable. Government payers, such as Medicare and
Medicaid, as well as insurers and larger employers have taken steps and may continue to take steps to control
the cost, utilization and delivery of healthcare services, including clinical laboratory services. Principally as a
result of reimbursement reductions and measures adopted by the Centers for Medicare & Medicaid Services, or
CMS (formerly the Health Care Financing Administration) which establishes procedures and continuously
evaluates and implements changes in the reimbursement process to control utilization, the percentage of our
aggregate net revenues derived from Medicare and Medicaid programs declined from approximately 20% in
1995 to approximately 17% in 2003. Despite the added cost and complexity of participating in the Medicare
and Medicaid programs, we continue to participate in such programs because we believe that our other business
may significantly depend on continued participation in the Medicare and Medicaid programs, because many
customers want a single laboratory to perform all of their clinical laboratory testing services, regardless of who
pays for such services.
Health insurers, which typically contract with a limited number of clinical laboratories for their members,
represent approximately one-half of our total testing volumes and one-half of our net revenues. Larger health
insurers typically prefer to use large commercial clinical laboratories because they can provide services on a
national or regional basis and can manage networks of local or regional laboratories to provide even broader
access to their members and physicians. In certain markets, such as California, health insurers delegate their
covered members to independent physician associations, or IPA, which in turn contract with laboratories for
clinical laboratory services.
Over the last decade, health insurers have been consolidating, resulting in fewer but larger insurers with
significant bargaining power to negotiate fee arrangements with healthcare providers, including clinical
laboratories. These health insurers demand that clinical laboratory service providers accept discounted fee
structures or assume all or a portion of the financial risk associated with providing testing services to their
members through capitated payment contracts. Under these capitated payment contracts, the Company and health
insurers agree to a predetermined monthly contractual rate for each member of the health insurer’s plan
regardless of the number or cost of services provided by the Company. Capitated agreements have historically
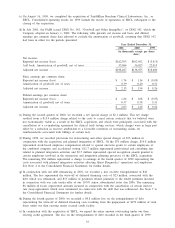
been priced aggressively, particularly for exclusive or semi-exclusive arrangements. In 2003, we derived
approximately 14% of our testing volume and 8% of our net revenues from capitated payment contracts. In
recent years, there has been a shift in the way major insurers contract with clinical laboratories. Health insurers
have begun to offer more freedom of choice to their affiliated physicians, including greater freedom to
determine which laboratory to use and which tests to order. Accordingly, most of our agreements with major
health insurers are non-exclusive arrangements. As a result, under these non-exclusive arrangements, physicians
have more freedom of choice in selecting laboratories, and laboratories are likely to compete more on the basis
of service and quality rather than price alone. Also, health insurers have been giving patients greater freedom of
choice and patients have increasingly been selecting plans (such as preferred provider organizations and
consumer driven plans) that offer a greater choice of providers. Pricing for these preferred provider
organizations is typically negotiated on a fee-for-service basis, which generally results in higher revenue per
requisition than under a capitated fee arrangement. Despite these trends, health insurers continue to aggressively
seek cost reductions in order to keep their premiums to their customers competitive.
We expect that the overall reimbursement dynamics for all payers on a combined basis are neutral for the
diagnostic testing industry. Today, many federal and state governments face serious budget deficits and
healthcare spending is a prime target for reductions. For example, the Prescription Drug, Improvement, and
Modernization Act of 2003 eliminated for five years (beginning January 1, 2004) the provision for annual
increases to the Medicare national fee schedule based on the consumer price index. Efforts to impose reduced
reimbursements and more stringent cost controls by government and other payers for existing tests may
continue. However, we believe that as new tests are developed which either improve on the effectiveness of
existing tests or provide new diagnostic capabilities, government and other payers will add these tests as
covered services, because of the importance of laboratory testing in assessing and managing the health of
patients. We continue to emphasize the importance and the high value of laboratory testing with insurers and
government payers at the federal and state level.
The diagnostic testing industry is subject to seasonal fluctuations in operating results and cash flows.
Typically, testing volume declines during the summer months, year-end holiday periods and other major
holidays, reducing net revenues and operating cash flows below annual averages. Testing volume is also subject
to declines in winter months due to inclement weather, which varies in severity from year to year.
38