Quest Diagnostics 2003 Annual Report Download - page 24
Download and view the complete annual report
Please find page 24 of the 2003 Quest Diagnostics annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
Payers and Customers
We provide testing services to a broad range of healthcare providers. We consider a “payer’’ as the party
that pays for the test and a “customer’’ as the party who refers the test to us. Depending on the billing
arrangement and applicable law, the payer may be (1) the physician or other party (such as another laboratory
or an employer) who referred the testing to us, (2) the patient, or (3) a third party who pays the bill for the
patient, such as an insurance company, Medicare or Medicaid. Some states, including New York, New Jersey
and Rhode Island, prohibit us from billing physician clients. We consider a managed care organization as both
our customer and a payer, when it contracts with us on an exclusive or semi-exclusive basis on behalf of its
patients.
During 2003, only two customers accounted for more than 5% of our net revenues, and no single customer
accounted for more than 7% of our net revenues. We believe that the loss of any one of our customers would
not have a material adverse effect on our financial condition, results of operations or cash flows.
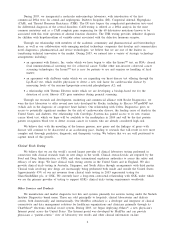
Payers
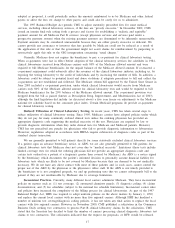
The following table shows current estimates of the breakdown of the percentage of our total volume of
requisitions and total clinical laboratory net revenues during 2003 applicable to each payer group:
Net Revenues as
% of
Requisition Volume Total Clinical
as % of Laboratory Net
Total Volume Revenues
Patient ................................................... 2%– 5% 5%–10%
Medicare and Medicaid ................................... 15%–20% 15%–20%
Physicians, Hospitals, Employers and Other Monthly-Billed
Payers ................................................. 35%–40% 20%–25%
Third Party Fee-for-Service ................................ 30%–35% 40%–45%
Managed Care-Capitated ................................... 10%–15% 5%–10%
Customers
Physicians
Physicians requiring testing for patients are the primary source of our clinical laboratory testing volume.
We typically bill physician accounts on a fee-for-service basis. Fees billed to physicians are based on the
laboratory’s client fee schedule and are typically negotiated. Fees billed to patients and insurance companies are
based on the laboratory’s patient fee schedule, subject to any limitations on fees negotiated with the insurance
companies or with physicians on behalf of their patients. Medicare and Medicaid reimbursements are based on
fee schedules set by governmental authorities.
Managed Care Organizations and Other Insurance Providers
Health insurers, which typically contract with a limited number of clinical laboratories for their members,
represent approximately one-half of our total testing volumes and one-half of our net revenues. Larger health
insurers typically prefer to use large commercial clinical laboratories because they can provide services on a
national or regional basis and can manage networks of local or regional laboratories to provide even broader
access to their members and physicians. In addition, larger laboratories are better able to achieve the low-cost
structures necessary to profitably service large health insurers and can provide test utilization data across their
various plans in a consistent format. In certain markets, such as California, many health insurers delegate their
covered members to independent physician associations, which in turn contract with laboratories for clinical
laboratory services.
Over the last decade, health insurers have been consolidating, resulting in fewer but larger insurers with
significant bargaining power in negotiating fee arrangements with healthcare providers, including clinical
laboratories. These health insurers demand that clinical laboratory service providers accept discounted fee
structures or assume all or a portion of the financial risk associated with providing testing services to their
members through capitated payment contracts. Under these capitated payment contracts, the Company and health
insurers agree to a predetermined monthly contractual rate for each member of the health insurer’s plan
regardless of the number or cost of services provided by the Company. Some services, such as various esoteric
tests, new technologies and anatomic pathology services, may be carved out from a capitated rate and, if carved
7