Quest Diagnostics 2003 Annual Report Download - page 54
Download and view the complete annual report
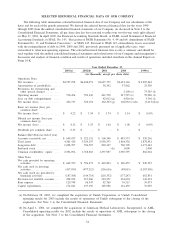
Please find page 54 of the 2003 Quest Diagnostics annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.QUEST DIAGNOSTICS INCORPORATED AND SUBSIDIARIES
MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION
AND RESULTS OF OPERATIONS
Overview
The underlying fundamentals of the diagnostic testing industry have improved since the early to mid-1990s,
which was a period of declining reimbursement and reduced test utilization. During the early 1990s, the
industry was negatively impacted by significant government regulation and investigations into various billing
practices. In addition, the rapid growth of managed care, as a result of the need to reduce overall healthcare
costs, and excess laboratory testing capacity, led to revenue and profit declines across the diagnostic testing
industry, which in turn led to industry consolidation, particularly among commercial laboratories. As a result of
these dynamics, fewer but larger commercial laboratories have emerged, which have greater economies of scale,
rigorous programs designed to assure compliance with government billing regulations and other laws, and a
more disciplined approach to pricing services. These changes have resulted in improved profitability and a
reduced risk of non-compliance with complex government regulations. At the same time, a slowdown in the
growth of managed care and decreasing influence by managed care organizations on the ordering of clinical
laboratory testing by physicians has contributed to renewed growth in testing and further improvements in
profitability since 1999. Partially offsetting these favorable trends have been changes in the United States
economy during the last several years, which has resulted in an increase in the number of unemployed and
uninsured. In addition, in an attempt to slow the rapidly rising costs of healthcare, employers and healthcare
insurers have made design changes to healthcare plans, which shift a larger portion of healthcare costs to
consumers. We believe that these factors have reduced the utilization of healthcare services in general. Orders
for laboratory testing are generated from physician offices, hospitals and employers. As such, factors such as the
number of unemployed and uninsured and design changes in healthcare plans, which impact the level of
employment or the number of physicians office and hospital visits, will impact the utilization of laboratory
testing.
We believe the diagnostic testing industry has continued to grow during the last several years despite the
slowdown in the United States economy and the changes in healthcare plan design, and that growth will
accelerate as the economy improves. In addition, over the longer term, growth is expected to accelerate as a
result of the following factors:
•general expansion and aging of the United States population;
•continuing research and development in the area of genomics and proteomics, which is expected to yield
new, more sophisticated and specialized diagnostics tests;
•increasing recognition by consumers and payers of the value of early detection and prevention which can
be provided through laboratory testing as a means to improve health and reduce the overall cost of
healthcare; and
•increasing affordability of tests due to advances in technology and cost efficiencies.
Quest Diagnostics, as the largest clinical laboratory testing company with a leading position in most of its
geographic markets and service offerings, is well positioned to benefit from the growth expected in the industry.
Payments for clinical laboratory testing services are made by the government, health insurers, physicians,
hospitals, employers and patients. Physicians, hospitals and employers are typically billed on a fee-for-service
basis based on fee schedules, which are typically negotiated. Fees billed to patients and health insurers are
based on the laboratory’s patient fee schedule, subject to any limitations on fees negotiated with the health
insurers or with physicians on behalf of their patients. Medicare and Medicaid reimbursements are based on fee
schedules set by governmental authorities.
We incur significant additional costs as a result of our participation in Medicare and Medicaid programs, as
billing and reimbursement for clinical laboratory testing is subject to considerable and complex federal and state
regulations. These additional costs include those related to: (1) complexity added to our billing processes;
(2) training and education of our employees and customers; (3) compliance and legal costs; and (4) costs
related to, among other factors, medical necessity denials and advance beneficiary notices. Compliance with
applicable laws and regulations, as well as internal compliance policies and procedures, adds further complexity
and costs to the billing process. We have implemented “best practices’’ that have significantly improved our
billing and collection processes. These efforts, together with our Six Sigma and standardization initiatives, have
significantly reduced bad debt expense as a percentage of net revenues over the last several years. While the
37