Quest Diagnostics 2000 Annual Report Download - page 76
Download and view the complete annual report
Please find page 76 of the 2000 Quest Diagnostics annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.F-6
QUEST DIAGNOSTICS INCORPORATED AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands unless otherwise indicated)
1. DESCRIPTION OF BUSINESS
Quest Diagnostics Incorporated and its subsidiaries (“Quest Diagnostics” or the “Company”) is the largest
clinical laboratory testing business in the United States. Prior to January 1, 1997, Quest Diagnostics was a wholly owned
subsidiary of Corning Incorporated (“Corning”). On December 31, 1996, Corning distributed all of the outstanding
shares of common stock of the Company to the stockholders of Corning as part of the “Spin-Off Distribution”.
As the nation’s leading provider of diagnostic testing and related services for the healthcare industry, Quest
Diagnostics offers a broad range of clinical laboratory testing services to physicians, hospitals, managed care
organizations, employers, governmental institutions and other independent clinical laboratories. Quest Diagnostics has
the leading market share in clinical laboratory testing and esoteric testing, including molecular diagnostics, as well as
anatomic pathology services and testing for drugs of abuse. Through the Company’s national network of laboratories and
patient service centers, and its leading esoteric testing laboratory and development facility known as Nichols Institute,
Quest Diagnostics offers comprehensive and innovative diagnostic testing, information and related services used by
physicians and other healthcare customers to diagnose, treat and monitor diseases and other medical conditions. Quest
Diagnostics offers clinical testing and services to support clinical trials of new pharmaceuticals worldwide. Quest
Informatics collects and analyzes laboratory, pharmaceutical and other data to develop information products to help
pharmaceutical companies with their marketing and disease management efforts, as well as to help healthcare customers
better manage the health of their patients.
Quest Diagnostics currently processes over 100 million requisitions each year through its extensive network of
laboratories and patient service centers in virtually every major metropolitan area throughout the United States.
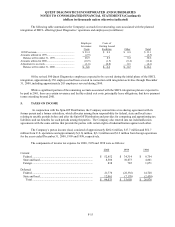
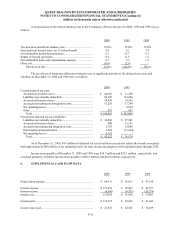
2. SUMMARY OF SIGNIFICANT ACCOUNTING POLICIES
Principles of Consolidation
The consolidated financial statements include the accounts of all entities controlled by the Company. The equity
method of accounting is used for investments in affiliates which are not Company controlled, and in which the
Company's interest is between 20 and 50 percent. The Company’s share of equity earnings (losses) from investments in
affiliates, accounted for under the equity method, totaled $5.5 million, $(0.7) million and $(5.2) million, respectively, for
2000, 1999 and 1998. The Company’s share of equity earnings (losses) is included in other, net in the consolidated
statements of operations. All significant intercompany accounts and transactions are eliminated.
Use of Estimates
The preparation of financial statements in conformity with accounting principles generally accepted in the
United States of America requires management to make estimates and assumptions that affect the reported amounts of
assets and liabilities and disclosure of contingent assets and liabilities at the date of the financial statements and the
reported amounts of revenues and expenses during the reporting period. Actual results could differ from those estimates.
Revenue Recognition
The Company generally recognizes revenue for services rendered upon completion of the testing process.
Billings for services under third-party payer programs, including Medicare and Medicaid, are recorded as revenues net of
allowances for differences between amounts billed and the estimated receipts under such programs. Adjustments to the
estimated receipts, based on final settlement with the third-party payers, are recorded upon settlement. In 2000, 1999 and
1998, approximately 13%, 14% and 16%, respectively, of net revenues were generated by Medicare and Medicaid
programs. Under capitated agreements with managed care customers, the Company recognizes revenue based on a
predetermined monthly contractual rate for each member of the managed care plan regardless of the number or cost of
services provided by the Company.