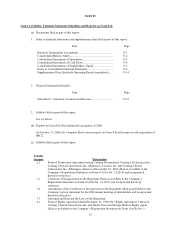
Quest Diagnostics 2000 Annual Report Download - page 36
Download and view the complete annual report
Please find page 36 of the 2000 Quest Diagnostics annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.16
Reduced Utilization of Clinical Laboratory Testing. In recent years, HCFA has taken several steps to reduce
utilization of clinical laboratory testing. Since 1995, Medicare carriers have adopted policies under which they do not
pay for many commonly ordered clinical tests unless the ordering physician has provided an appropriate diagnostic code
supporting the medical necessity of the test. Physicians are required by law to provide diagnostic information when they
order clinical tests for Medicare and Medicaid patients. However, there is no penalty prescribed for violations of this
law.
In March 1996, HCFA eliminated its prior policy under which Medicare paid for all tests contained in an
automated chemistry panel when at least one of the tests in the panel is medically necessary. HCFA indicated that under
the new policy, Medicare will only pay for those individual tests in a chemistry panel that are medically necessary.
Subsequently the American Medical Association (“AMA”), in conjunction with HCFA, eliminated the existing
automated chemistry panel series (CPT Codes 80002-80019) and designated four new panels of “clinically relevant”
automated chemistry panels. HCFA adopted these panels in 1998, and in 1999 and 2000 amended these new panels or
created additional panels.
We are generally permitted to bill patients directly for some statutorily excluded clinical laboratory services. We
are also generally permitted to bill patients for clinical laboratory tests that Medicare does not pay for due to “medical
necessity” limitations (these tests include limited coverage tests for which a carrier-approved diagnosis code is not
provided by the ordering physician) if the patient signs an advance beneficiary notice (ABN). See “Billing”.
Inconsistent Practices. Currently, many different local carriers administer Medicare. They have inconsistent
policies on matters such as: (1) test coverage; (2) automated chemistry panels; (3) diagnosis coding; (4) claims
documentation; and (5) fee schedules (subject to the national limitations). Inconsistent regulation has increased the
complexity of the billing process for clinical laboratories. As part of the 1997 Balanced Budget Act, HHS was required
to adopt uniform policies on the above matters by January 1, 1999 and replace the current local carriers with no more
than five regional carriers. Although HHS has finalized a number of uniform policies, it has not taken any final action to
replace the local carriers with five regional carriers. However, in November 2000, HCFA published a solicitation in the
Commerce Business Daily seeking two contractors to process Part B clinical laboratory claims. In the solicitation, HCFA
stated that the Secretary has decided to limit the number of carriers processing clinical diagnostic laboratory test claims to
two contractors. The solicitation indicated that the Request for Proposal (RFP) would be released on or before December
31, 2000 but as of March 14, 2001, it had not been issued; the solicitation did not indicate the effective date for a final
transition to the regional carrier model.
HCFA plans to achieve standardization through the help of a single claims processing system for all carriers.
This initiative, however, was suspended due to HCFA’s Year 2000 compliance priorities.
Competitive Bidding. The 1997 Balanced Budget Act requires HCFA to conduct five Medicare bidding
demonstrations involving various types of medical services and complete them by 2002. HCFA is expected to include a
clinical laboratory demonstration project in a metropolitan statistical area as part of the legislative mandate. If
competitive bidding were implemented on a regional or national basis for clinical laboratory testing, it could materially
adversely affect the clinical laboratory industry and us.
Future Legislation. Future changes in federal, state and local regulations (or in the interpretation of current
regulations) affecting governmental reimbursement for clinical laboratory testing could adversely affect us. We cannot
predict, however, whether and what type of legislative proposals will be enacted into law or what regulations will be
adopted by regulatory authorities.
Fraud and Abuse Regulations. Medicare and Medicaid anti-kickback laws prohibit clinical laboratories from
making payments or furnishing other benefits to influence the referral of tests billed to Medicare, Medicaid or other
federal programs.
Various federal enforcement agencies, including the Federal Bureau of Investigations (“FBI”) and the OIG,
liberally interpret and aggressively enforce statutory fraud and abuse provisions. According to public statements by the
Department of Justice (“DOJ”), during the last several years healthcare fraud has been elevated to one of the highest
priorities of the DOJ, and substantial prosecutorial and other law enforcement resources have been committed to
investigating healthcare provider fraud. The OIG also is involved in investigations of healthcare fraud and has, according
to recent workplans, targeted certain laboratory practices for study, investigation and prosecution. As noted above, the
penalties for violation of these laws may include criminal and civil fines and penalties and exclusion from participation in
federal programs. Many of the anti-fraud statutes and regulations, including those relating to joint ventures and