Express Scripts 2013 Annual Report Download - page 8
Download and view the complete annual report
Please find page 8 of the 2013 Express Scripts annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
Express Scripts 2013 Annual Report 8
Products and Services
Pharmacy Benefit Management Services
Overview. Our core PBM services involve the management of outpatient prescription drug utilization to foster high
quality, cost-effective pharmaceutical care. We consult with our clients to assist in the selection of plan design features that
balance clients’ requirements for cost control with member choice and convenience. We focus our solutions to enable better
decisions in four important and interrelated areas: benefit choices, drug choices, pharmacy choices and health choices. As a
result of these solutions, we believe we are able to deliver healthier outcomes, higher member satisfaction and a more
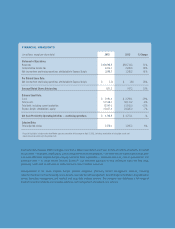
affordable prescription drug benefit. During 2013, 97.9% of our revenue was derived from our PBM operations, compared to
97.6% and 97.2% during 2012 and 2011, respectively.
Retail Network Pharmacy Administration. We contract with retail pharmacies to provide prescription drugs to
members of the pharmacy benefit plans we manage. In the United States, Puerto Rico and the Virgin Islands, we negotiate with
pharmacies to discount the price at which they will provide drugs to members and manage national and regional networks that
are responsive to client preferences related to cost containment, convenience of access for members and network performance.
We also manage networks of pharmacies that are customized for or under direct contract with specific clients. In addition, we
have contracted Medicare Part D provider networks to comply with CMS access requirements for the Medicare Part D
Prescription Drug Program (“PDP”).
All retail pharmacies in our pharmacy networks communicate with us online and in real time to process
prescription drug claims. When a member of a plan presents his or her identification card at a network pharmacy, the network
pharmacist sends certain specified member, prescriber and prescription information in an industry-standard format through our
systems, which process the claim and send a response back to the pharmacy.
Home Delivery Pharmacy Services. We also dispense prescription drugs from our five high-volume automated
dispensing home delivery pharmacies and one non-automated dispensing home delivery pharmacy. In addition to the order
processing that occurs at these home delivery pharmacies, we also operate several non-dispensing order processing facilities
and patient contact centers. We also maintain one non-dispensing home delivery fulfillment pharmacy for business continuity
purposes. Our pharmacies provide patients with convenient access to maintenance medications and enable us to manage our
clients’ drug costs through operating efficiencies and economies of scale as well as provide greater safety and accuracy.
Through our home delivery pharmacies, we are directly involved with the prescriber and patient and, as a result, research
shows we are generally able to achieve a higher level of generic substitutions, therapeutic interventions and better adherence
than can be achieved through the retail pharmacy networks.
Benefit Design Consultation. We provide clinically sound formularies that encourage the use of equally effective
but lower-cost drugs over higher-cost alternatives. This is accomplished through formulary compliance strategies that also
maintain member satisfaction. Express Scripts offers several base and advanced formulary management options for clients,
including Medicare Part D and Public Exchange formularies. We also offer clients a variety of utilization management tools to
manage patient drug utilization and overall drug spend. The most common benefit design options we offer to our clients are
financial incentives and reimbursement limitations on the drugs covered by the plan, including drug formularies, tiered co-
payments, deductibles or annual benefit maximums, as well as utilization management programs.
Drug Utilization Review. Our electronic claims processing system enables us to implement sophisticated
intervention programs to assist in managing prescription drug utilization. The system can alert the pharmacist to drug safety
concerns, generic substitution and therapeutic intervention opportunities, as well as formulary adherence issues, and can also
administer prior authorization, step therapy protocol programs and drug quantity management at the time a claim is submitted
for processing. Our claims processing system also creates a database of drug utilization information that can be accessed at the
time the prescription is dispensed, on a retrospective basis to analyze utilization trends and prescribing patterns for more
intensive management of the drug benefit, and on a prospective basis to help support pharmacists in drug therapy management
decisions.
Drug Formulary Management. Formularies are lists of drugs to which benefit design is applied under the
applicable plan. Formulary management enables patients and physicians to choose clinically appropriate and cost-effective
drugs for a given condition. Our foremost consideration in the formulary development process is the clinical appropriateness of
the particular drugs. In developing formularies, we first perform a rigorous assessment of the available evidence regarding each
drug’s safety and clinical effectiveness. No new drug is added to the formulary until it meets standards of quality established by
our National Pharmacy & Therapeutics (“P&T”) Committee, a panel composed of 16 independent physicians and pharmacists
in active clinical practice, representing a variety of specialties and practice settings, typically with major academic affiliations.
We fully comply with the P&T Committee’s clinical recommendations. In making its clinical recommendation, the P&T
Committee has no information regarding the discount or rebate arrangement we might negotiate with the manufacturer. This is