Express Scripts 2013 Annual Report Download - page 68
Download and view the complete annual report
Please find page 68 of the 2013 Express Scripts annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
Express Scripts 2013 Annual Report 68
percentages. These estimates are adjusted to actual when amounts are paid to clients subsequent to collections from
pharmaceutical manufacturers. We record rebates and administrative fees receivable from the manufacturer and payable to
clients when the prescriptions covered under contractual agreements with the manufacturers are dispensed; these amounts are
not dependent upon future pharmaceutical sales. Rebates and administrative fees billed to manufacturers are determinable when
the drug is dispensed. We pay all or a contractually agreed upon portion of such rebates to our clients.
We also administer Medco’s market share performance rebate program. Estimates for rebates receivable and the
related amounts payable to clients are accrued monthly based on the terms of the applicable contract, historical data and current
utilization. These estimates are adjusted to actual when amounts are paid to clients subsequent to collections from
pharmaceutical manufacturers.
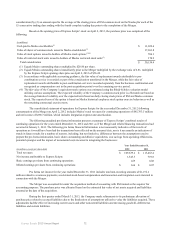
Medicare prescription drug program. Our revenues include premiums associated with our Medicare prescription
drug program (“PDP”) risk-based product offerings. These products involve prescription dispensing for beneficiaries enrolled
in the Centers for Medicare & Medicaid Services (“CMS”)-sponsored Medicare Part D Prescription Drug Program (“Medicare
Part D”) prescription drug benefit. We also offer numerous customized benefit plan designs to employer group retiree plans
under the Medicare Part D prescription drug benefit.
The PDP premiums are determined based on our annual bid and related contractual arrangements with CMS. The
PDP premiums are primarily comprised of amounts received from CMS as part of a direct subsidy and an additional subsidy
from CMS for low-income member premiums, as well as premium payments received from members. These premiums are
recognized ratably to revenues over the period in which members are entitled to receive benefits. Premiums received in
advance of the applicable benefit period are deferred and recorded in accrued expenses on the consolidated balance sheet.
There is a possibility that the annual costs of drugs may be higher or lower than premium revenues. As a result, CMS provides
a risk corridor adjustment for the standard drug benefit that compares our actual annual drug costs incurred to the targeted
premiums in our CMS-approved bid. Based on the risk corridor, we will receive from CMS additional premium amounts or be
required to refund to CMS previously received premium amounts. We calculate the risk corridor adjustment on a quarterly basis
based on drug cost experience to date and record an adjustment to revenues with a corresponding receivable from or payable to
CMS reflected on the consolidated balance sheet.
In addition to PDP premiums, there are certain co-payments and deductibles (the “cost share”) due from members
based on prescription orders by those members, some of which are subsidized by CMS in cases of low-income membership.
Non-low-income members received a cost share benefit under the coverage gap discount program with brand pharmaceutical
manufacturers. For subsidies received in advance, the amount is deferred and recorded in accrued expenses on the consolidated
balance sheet. If there is cost share due from members, pharmaceutical manufacturers or CMS, or premiums due from
members, the amount is accrued and recorded in receivables, net, on the consolidated balance sheet. After the end of the
contract year and based on actual annual drug costs incurred, cost share amounts are reconciled with CMS and the
corresponding receivable or payable is settled. The cost share is treated consistently as other co-payments derived from
providing PBM services, a component of revenues on the consolidated statement of operations.
Our cost of revenues includes the cost of drugs dispensed by our home delivery pharmacies or retail network for
members covered under our Medicare PDP product offerings. These amounts are recorded at cost as incurred. We receive a
catastrophic reinsurance subsidy from CMS for approximately 80% of costs incurred by individual members in excess of the
individual annual out-of-pocket maximum. The subsidy is reflected as an offsetting credit in cost of revenues to the extent that
catastrophic costs are incurred. Catastrophic reinsurance subsidy amounts received in advance are deferred and recorded in
accrued expenses on the consolidated balance sheet. If there are catastrophic reinsurance subsidies due from CMS, the amount
is accrued and recorded in receivables, net, on the consolidated balance sheet. After the end of the contract year and based on
actual annual drug costs incurred, catastrophic reinsurance amounts are reconciled with CMS and the corresponding receivable
or payable is settled.
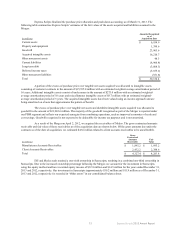
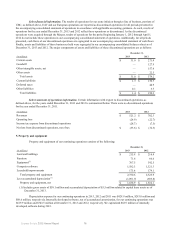
Cost of revenues. Cost of revenues includes product costs, network pharmacy claims costs, co-payments and other
direct costs associated with dispensing prescriptions, including shipping and handling (see also “Revenue recognition” and
“Rebate accounting”).
Surescripts. Surescripts enables physicians to securely access health information when caring for their patients
through a fast and efficient health exchange. ESI and Medco each retained a one-sixth ownership in Surescripts, resulting in a
combined one-third ownership in Surescripts. Due to the increased ownership percentage following the Merger, we account for
the investment in Surescripts using the equity method. See Note 3 - Changes in business for further information.
Income taxes. Deferred tax assets and liabilities are recognized based on temporary differences between financial
statement basis and tax basis of assets and liabilities using presently enacted tax rates. We account for uncertainty in income
taxes as described in Note 8 - Income taxes.