Express Scripts 2012 Annual Report Download - page 64
Download and view the complete annual report
Please find page 64 of the 2012 Express Scripts annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Express Scripts 2012 Annual Report62
networks, and providing services to drug manufacturers, including administration of discount programs (see also
“Rebate accounting” below).
Revenues from dispensing prescriptions from our home delivery pharmacies are recorded when drugs are
shipped. At the time of shipment, our earnings process is complete; the obligation of our customer to pay for the
drugs is fixed and, due to the nature of the product, the member may not return the drugs nor receive a refund.
Revenues from our specialty line of business are from providing medications/pharmaceuticals for diseases
that rely upon high-cost injectable, infused, oral or inhaled drugs which have sensitive handling and storage needs,
bio-pharmaceutical services including marketing, reimbursement, customized logistics solutions and providing
fertility services to providers and patients. Specialty revenues earned by our PBM segment are recognized at the
point of shipment. At the time of shipment, we have performed substantially all of our obligations under our
customer contracts and do not experience a significant level of reshipments. Appropriate reserves are recorded for
discounts and contractual allowances which are estimated based on historical collections over a recent period. Any
differences between our estimates and actual collections are reflected in operations in the period in which payment is
received. Differences may affect the amount and timing of our revenues for any period if actual performance varies
from our estimates. Allowances for returns are estimated based on historical return trends.
Revenues from our PBM segment are also derived from the distribution of pharmaceuticals requiring
special handling or packaging where we have been selected by the pharmaceutical manufacturer as part of a limited
distribution network and the distribution of pharmaceuticals through Patient Assistance Programs where we receive
a fee from the pharmaceutical manufacturer for administrative and pharmacy services for the delivery of certain
drugs free of charge to doctors for their low-income patients. These revenues include administrative fees received
from these programs.
Revenues related to the distribution of prescription drugs by retail pharmacies in our networks consist of
the prescription price (ingredient cost plus dispensing fee) negotiated with our clients, including the portion to be
settled directly by the member (co-payment), plus any associated administrative fees. These revenues are recognized
when the claim is processed. When we independently have a contractual obligation to pay our network pharmacy
providers for benefits provided to our clients’ members, we act as a principal in the arrangement and we include the
total prescription price as revenue in accordance with applicable accounting guidance. Although we generally do not
have credit risk with respect to retail co-payments, the primary indicators of gross treatment are present. When a
prescription is presented by a member to a retail pharmacy within our network, we are solely responsible for
confirming member eligibility, performing drug utilization review, reviewing for drug-to-drug interactions,
performing clinical intervention, which may involve a call to the member’s physician, communicating plan
provisions to the pharmacy, directing payment to the pharmacy and billing the client for the amount it is
contractually obligated to pay us for the prescription dispensed, as specified within our client contracts. We also
provide benefit design and formulary consultation services to clients. We have separately negotiated contractual
relationships with our clients and with network pharmacies, and under our contracts with pharmacies we assume the
credit risk of our clients’ ability to pay for drugs dispensed by these pharmacies to clients’ members. We, not our
clients, are obligated to pay the retail pharmacies in our networks the contractually agreed upon amount for the
prescription dispensed, as specified within our provider contracts. These factors indicate we are a principal as
defined by applicable accounting guidance and, as such, we record the total prescription price contracted with clients
in revenue.
If we merely administer a client’s network pharmacy contracts to which we are not a party and under which
we do not assume credit risk, we record only our administrative fees as revenue. For these clients, we earn an
administrative fee for collecting payments from the client and remitting the corresponding amount to the pharmacies
in the client’s network. In these transactions we act as a conduit for the client. Because we are not the principal in
these transactions, drug ingredient cost is not included in our revenues or in our cost of revenues.
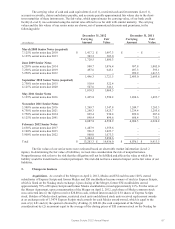
In retail pharmacy transactions, amounts paid to pharmacies and amounts charged to clients are always
exclusive of the applicable co-payment. Retail pharmacy co-payments, which we instructed retail pharmacies to
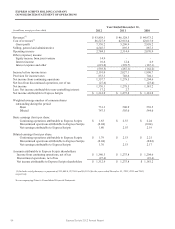
collect from members, of $11.7 billion, $5.8 billion and $6.2 billion for the years ended December 31, 2012, 2011
and 2010, respectively, are included in revenues and cost of revenues. Retail pharmacy co-payments increased in the
year ended December 31, 2012 as compared to 2011 due to the Merger.
Many of our contracts contain terms whereby we make certain financial and performance guarantees,
including the minimum level of discounts or rebates a client may receive, generic utilization rates and various
service guarantees. These clients may be entitled to performance penalties if we fail to meet a financial or service