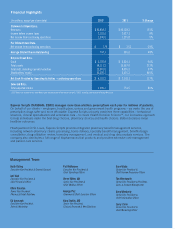
Express Scripts 2012 Annual Report Download - page 6
Download and view the complete annual report
Please find page 6 of the 2012 Express Scripts annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Express Scripts 2012 Annual Report4
Products and Services
Pharmacy Benefit Management Services
Overview. Our PBM services involve the management of outpatient prescription drug utilization to foster high
quality, cost-effective pharmaceutical care. We consult with our clients to assist them in selecting plan design features that
balance clients’ requirements for cost control with member choice and convenience. Our direct relationship with patients
also enables us to leverage the principles of Health Decision Science, our proprietary approach that combines the
behavioral sciences, clinical specialization and actionable data to help patients make better decisions about their health and
the cost of their care. As a result of these interactions, we believe we are able to deliver healthier outcomes, higher member
satisfaction and a more affordable prescription drug benefit. During 2012, 97.6% of our revenue was derived by our PBM
operations, compared to 97.2% and 97.4% during 2011 and 2010, respectively.
Retail Network Pharmacy Administration. We contract with retail pharmacies to provide prescription drugs to
members of the pharmacy benefit plans we manage. In the United States, Puerto Rico and the Virgin Islands, we negotiate
with pharmacies to discount the price at which they will provide drugs to members and manage national and regional
networks that are responsive to client preferences related to cost containment, convenience of access for members and
network performance. We also manage networks of pharmacies that are customized for or under direct contract with
specific clients. In addition, we have contracted Medicare Part D provider networks to comply with CMS access
requirements for the Medicare Part D Prescription Drug Program.
All retail pharmacies in our pharmacy networks communicate with us online and in real time to process
prescription drug claims. When a member of a plan presents his or her identification card at a network pharmacy, the
network pharmacist sends certain specified member, prescriber, and prescription information in an industry-standard format
through our systems, which process the claim and send a response back to the pharmacy. The electronic processing of the
claim includes, among other things, the following:
Q confirming the member’s eligibility for benefits under the applicable health benefit plan and any conditions or
limitations on coverage
Q performing a concurrent drug utilization review and alerting the pharmacist to possible drug interactions and
reactions or other indications of inappropriate prescription drug usage
Q updating the member’s prescription drug claim record
Q if the claim is accepted, confirming to the pharmacy that it will receive payment for the drug dispensed according
to its provider agreement with us
Q informing the pharmacy of the co-payment amount to be collected from the member based upon the client’s plan
design and the remaining payable amount due to the pharmacy
Home Delivery Services. As of December 31, 2012, we dispensed prescription drugs from our five high-volume
automated dispensing home delivery pharmacies and one non-automated dispensing home delivery pharmacy. In addition
to the order processing that occurs at these home delivery pharmacies, we also operate several non-dispensing order
processing facilities and patient contact centers. We also maintain one non-dispensing home delivery fulfillment pharmacy
for business continuity purposes. Our pharmacies provide patients with convenient access to maintenance medications and
enable us to manage our clients’ drug costs through operating efficiencies and economies of scale as well as provide greater
safety and accuracy. Through our home delivery pharmacies, we are directly involved with the prescriber and patient and,
as a result, research shows we are generally able to achieve a higher level of generic substitutions, therapeutic interventions
and better adherence than can be achieved through the retail pharmacy networks.
Benefit Design Consultation. We offer consultation and financial modeling to assist our clients in selecting benefit
plan designs that meet their needs for member satisfaction and cost control. The most common benefit design options we
offer to our clients are:
Q financial incentives and reimbursement limitations on the drugs covered by the plan, including drug formularies,
tiered co-payments, deductibles or annual benefit maximums
Q generic drug utilization incentives
Q incentives or requirements to use only certain network pharmacies or to order certain maintenance drugs (e.g.,
therapies for diabetes, high blood pressure, etc.) only through our home delivery pharmacies
Q reimbursement limitations on the amount of a drug that can be obtained in a specific period
Q utilization management programs such as step therapy and prior authorization, which focus the use of medications
according to clinically developed algorithms
Q
Q
Q
Q
Q