Cigna 2015 Annual Report Download - page 34
Download and view the complete annual report
Please find page 34 of the 2015 Cigna annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.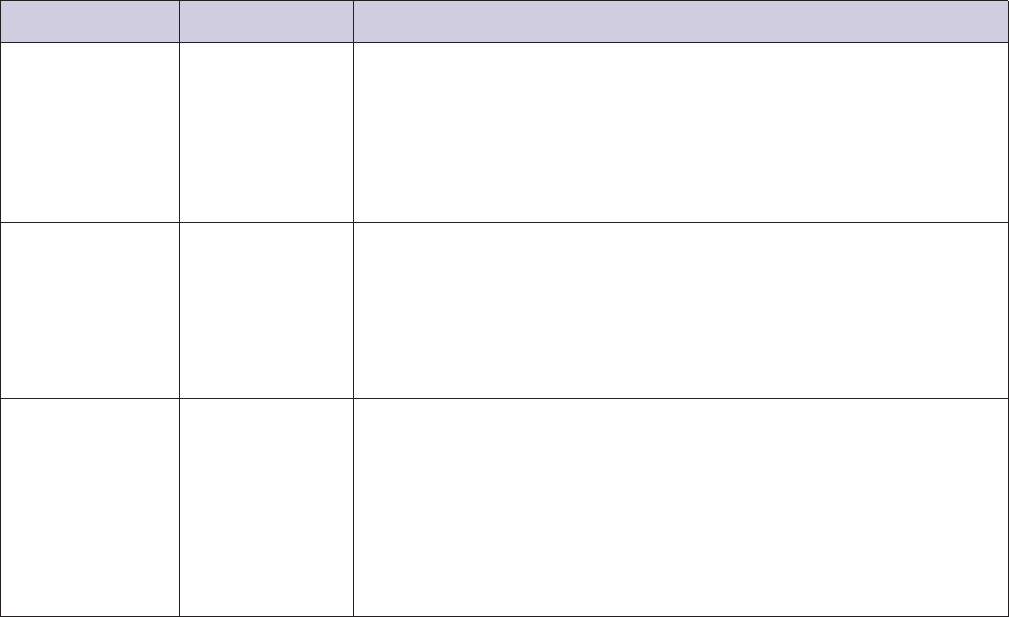
PART I
ITEM 1. Business
customer’s cost-sharing obligation is usually greater for the
Principal Products and Services
out-of-network care.
Commercial Medical Health Plans – U.S. and
•PPO Plans. Our PPO product line features a network with broader
International
provider access than the Managed Care Plans. The preferred
provider product line may be at a higher medical cost than our
The Commercial operating segment, either directly or through its
Managed Care Plans.
partners, offers some or all of its products in all 50 states, the District
of Columbia, the U.S. Virgin Islands, Canada, Europe, the Middle •Choice Fund Suite of Consumer-Driven Products. Our medical
East, and Asia. We offer a variety of medical plans including: plans are often integrated with the Cigna Choice Fund suite of
products: Health Reimbursement Accounts (‘‘HRA’’), Health
•Managed Care Plans including HMO, Network, Network Open Access
Savings Accounts (‘‘HSA’’) and Flexible Spending Accounts
and Open Access Plus. We offer health care services through Health
(‘‘FSA’’). These Choice Fund products are designed to encourage
Maintenance Organizations (‘‘HMOs’’) and insured and
customers to play an active role in understanding and managing
self-insured indemnity managed care benefit plans that use
their health and associated expenses. Customers can use these
meaningful cost-sharing incentives to encourage the use of
tax-advantaged accounts to finance eligible health care expenses and
‘‘in-network’’ versus ‘‘out-of-network’’ health care providers and
other approved services. In most cases, these products are combined
provide the option to select a primary care physician. The national
with a high deductible medical plan. We continue to experience
provider network for Managed Care Plans is somewhat smaller than
strong growth in these products and they represent a rapidly
the national network used with the preferred provider (‘‘PPO’’) plan
growing percentage of our overall medical customer base.
product line. If a particular plan covers non-emergency services
received from a non-participating health care provider, the
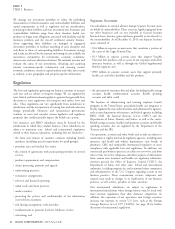
Approximately 90% of our commercial medical customers are enrolled in medical plans with funding arrangements that allow the corporate client
to directly benefit from lower medical costs. The funding arrangements available for our commercial medical and dental health plans are as
follows:
% of Commercial
Funding Arrangement Medical Customers Description
Administrative Services 83% ASO plan sponsors are responsible for self-funding all claims, but may purchase stop loss
Only (‘‘ASO’’) insurance to limit exposure for claims that exceed a predetermined amount.
We collect fees from plan sponsors for providing access to our participating provider network
and for other services and programs including: claims administration; behavioral health; disease
management; utilization management; cost containment; dental; and pharmacy benefit
management.
In some cases, we provide performance guarantees associated with meeting certain service
standards, clinical outcomes or financial metrics.
Insured – Experience 6% Premium charged during a policy period (‘‘initial premium’’) may be adjusted following the
Rated (‘‘Shared policy period for actual claim, and in some cases, administrative cost experience of the
Returns’’) policyholder:
When claims and expenses are less than the initial premium charged (an ‘‘experience
surplus’’), the policyholder may be credited for a portion of this premium.
However, if claims and expenses exceed the initial premium (an ‘‘experience deficit’’), we bear
these costs. In certain cases, experience deficits may be recovered through experience surpluses
in a future year if the policyholder renews.
Insured – Guaranteed 11% We establish the cost to the policyholder at the beginning of a policy period and generally
Cost cannot subsequently adjust premiums to reflect actual claim experience until the next annual
renewal.
Employers and other groups with guaranteed cost policies are generally smaller than those with
experience-rated group policies. Accordingly, our claim and expense assumptions may be based
in whole or in part on prior experience of the policyholder or on a pool of similar
policyholders.
HMO and individual plans (medical and dental) are offered on a guaranteed cost basis only.
Individual and ‘‘small employer’’ (employers with 50 or fewer employees) plans are required to
be community-rated under federal law.
We offer stop loss insurance coverage for ASO plans that provides In most states, individual and group insurance premium rates must be
reimbursement for claims in excess of a predetermined amount for approved by the applicable state regulatory agency (typically
individuals (‘‘specific’’), the entire group (‘‘aggregate’’), or both. In department of insurance) and state or federal laws may restrict or limit
addition, our experience-rated group medical insurance policies the use of rating methods. Premium rates for groups and individuals
include premium funding options similar to administrative services are subject to state review for reasonableness. In addition, Health Care
combined with stop loss coverage. Reform subjects individual and small group policy rate increases above
4 CIGNA CORPORATION - 2015 Form 10-K
•
•
•
•
•
•
•
•
•