CVS 2013 Annual Report Download - page 18
Download and view the complete annual report
Please find page 18 of the 2013 CVS annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
16
CVS Caremark
10-year agreement with Cardinal Health to form the
largest generic-sourcing entity in the United States. We
will collaborate with generic manufacturers to develop
innovative purchasing methodologies, improve supply
chain efficiencies, and use our compelling scale to
create attractive offerings for these suppliers.
The power of our integrated model has created a sus-
tainable competitive advantage for us. This is highlighted
by the growth of CVS/pharmacy’s share of our own
PBM’s retail network claims. That figure has jumped from
19 percent in 2008 – just following our merger – to
30 percent in 2013. This is a clear indicator that our
channel-agnostic approach is better positioned to cap-
ture share over the long-term, regardless of changes in
payor mix, plan design strategies, or patient preferences.
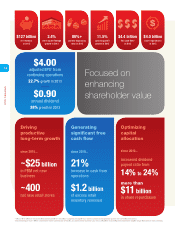
We generated $4.4 billion in free cash flow in 2013, and
we returned more than $5 billion to shareholders through
dividends and share repurchases. We increased our
quarterly dividend by 38 percent in 2013 and recently
announced another 22 percent increase for 2014,
which marks our 11th consecutive year of increases.
This recent dividend increase should allow us to achieve
a 25 percent payout ratio sometime this year, up from
14 percent in 2010. Looking forward, we recently set
a target payout ratio of 35 percent by 2018 as we
continue to focus on returning value to our shareholders.
Furthermore, after spending approximately $11 billion
on share repurchases from 2011 through 2013, our
board of directors recently authorized a new $6 billion
share repurchase program. Our current plans call for the
repurchase of approximately $4 billion of our shares in
2014, consistent with last year.
Our 2013 acquisitions of Drogaria Onofre and NovoLogix,
and of Coram, which closed in January 2014, offer good
examples of how we apply disciplined capital allocation
practices to supplement existing assets and bolster our
offerings. Drogaria Onofre, a 46-store retail drugstore
chain in Brazil, represents our first retail foray into the
international markets, while NovoLogix and Coram have
broadened our already compelling specialty solutions.
Our focus on enhancing shareholder value paid off
handsomely in 2013, with our shares producing a total
return to shareholders of 50.4 percent for the year. That
far surpassed the total returns of both the S&P 500
Index and Dow Jones Industrial Average over the same
period. We have outperformed these broader indices on
a three-, five-, and 10-year basis as well.
Our differentiated PBM offerings continue to
gain momentum
Our PBM business posted another strong year in
2013 with nice momentum heading into 2014. For the
2014 selling season, gross new business wins totaled
$5.3 billion. Factoring in a 96 percent retention rate,
we gained approximately $2.4 billion in client net new
business for 2014. Not reflected in that number is
$1.3 billion in lost revenue in 2014 resulting from last
year’s Medicare Part D sanction. I’m pleased to report
that the sanction was lifted on January 1, 2014, and
that we have once again started enrolling new members
into our SilverScript prescription drug plans (PDPs) as
they age into the Medicare program.
Although price is still a very important part of their
decision process, clients are telling us that we’re also
being selected because of the unique capabilities we
deliver. Among them, our Pharmacy Advisor® program
helps participating plan members with certain chronic
diseases, such as diabetes and cardiovascular condi-
tions, to identify gaps in care, adhere to their prescribed
medications, and better manage their health conditions.
We have also expanded this program to Medicare
beneficiaries, which is helping health plan clients achieve
better clinical star ratings.
Maintenance Choice® remains a unique offering in the
market that no competitor has been able to replicate.
It allows plan members to receive their 90-day mainte-
nance prescriptions by mail or at one of our convenient
retail stores for the same price. Client adoption has
risen significantly over the past two years, with 17 million
members currently enrolled, up 55 percent in that time
frame. Moreover, significant opportunity for growth
remains, with potential adoption among current clients
representing up to a total of 34 million members.
Regarding our long-term partnership with Aetna, we
have successfully completed the migration of Aetna’s
commercial membership to our destination platform.
Aetna’s Medicare Part D business will transition in