Quest Diagnostics 2005 Annual Report Download - page 41
Download and view the complete annual report
Please find page 41 of the 2005 Quest Diagnostics annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.material to our results of operations and cash flows in the period in which the impact of such matters is
determined or paid.
The Clinical Laboratory Improvement Amendments of 1988 (CLIA) regulates virtually all clinical
laboratories by requiring that they be certified by the federal government and comply with various operational,
personnel and quality requirements intended to ensure that their clinical laboratory testing services are accurate,
reliable and timely. Furthermore, CLIA does not preempt state laws that are more stringent than federal law.
Some state laws may require additional personnel qualifications, quality control, record maintenance and/or
proficiency testing. Intentional and serious failures to comply with these requirements can lead to loss of
licenses, exclusion from the Medicare and Medicaid programs, fines and other penalties.
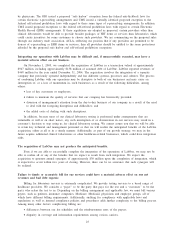
Billing and reimbursement for clinical laboratory testing is subject to significant and complex federal and
state regulation. Penalties for violations of laws relating to billing federal healthcare programs and for violations
of federal fraud and abuse laws include: (1) exclusion from participation in the Medicare/Medicaid programs;
(2) asset forfeitures; (3) civil and criminal fines and penalties; and (4) the loss of various licenses, certificates
and authorizations necessary to operate some or all of a clinical laboratory’s business. Civil monetary penalties
for a wide range of violations are not more than $10,000 per violation plus three times the amount claimed
and, in the case of kickback violations, not more than $50,000 per violation plus up to three times the amount
of remuneration involved. A parallel civil remedy under the federal False Claims Act provides for damages not
more than $11,000 per violation plus up to three times the amount claimed.
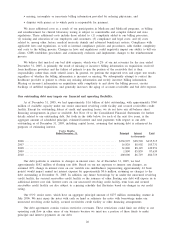
As an integral part of our compliance program, we investigate all reported or suspected failures to comply
with federal and state healthcare reimbursement requirements. Any non-compliance that results in Medicare or
Medicaid overpayments is reported to the government and reimbursed by us. As a result of these efforts, we
have periodically identified and reported overpayments. While we have reimbursed these overpayments and have
taken corrective action where appropriate, we cannot assure investors that in each instance the government will
necessarily accept these actions as sufficient.
Failure in our information technology systems, including failures resulting from our systems conversions
or failures to adapt existing systems to proposed Health Information Technology (HIT) standards, could
significantly increase turnaround time, otherwise disrupt our operations, or lead to increased competition
by other providers of laboratory services, all of which could reduce our customer base and result in lost
net revenues.
Information systems are used extensively in virtually all aspects of our business, including laboratory
testing, billing, customer service, logistics and management of medical data. Our success depends, in part, on
the continued and uninterrupted performance of our information technology, or IT, systems. IT systems are
vulnerable to damage from a variety of sources, including telecommunications or network failures, malicious
human acts and natural disasters. Moreover, despite network security measures, some of our servers are
potentially vulnerable to physical or electronic break-ins, computer viruses and similar disruptive problems.
Despite the precautionary measures we have taken to prevent unanticipated problems that could affect our IT
systems, sustained or repeated system failures that interrupt our ability to process test orders, deliver test results
or perform tests in a timely manner could adversely affect our reputation and result in a loss of customers and
net revenues.
During 2002, we began implementation of a standard laboratory information system and a standard billing
system. The deployment of standardized systems is continuing and we expect that it will take several years to
complete and will result in significantly more centralized systems than we have today. Failure to properly
implement this standardization process could materially adversely affect our business. During system conversions
of this type, workflow may be reengineered to take advantage of enhanced system capabilities, which may cause
temporary disruptions in service. In addition, the implementation process, including the transfer of databases and
master files to new data centers, presents significant conversion risks that need to be managed carefully.
In addition, public and private initiatives at the federal, state and regional levels to create HIT standards for
the electronic exchange of clinical information, including laboratory results, could require costly modifications to
our existing IT systems. While we do not expect HIT standards to be adopted or implemented without adequate
time to comply with new standards, failure or delay in implementing HIT interoperability standards or in
adopting and incorporating standardized clinical coding systems in our IT systems, could result in a loss of
customers, a loss of business opportunities, and could adversely affect our reputation. On October 11, 2005, the
OIG and CMS published separate NPRMs intended to create incentives to foster the quicker adoption of HIT
24