Quest Diagnostics 2009 Annual Report Download - page 20
Download and view the complete annual report
Please find page 20 of the 2009 Quest Diagnostics annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
Health information technologies. Demand is growing toward comprehensive care management solutions that
serve patients, payers and practitioners by improving access to patient data, increasing patient participation in care
management, reducing medical errors and improving clinical outcomes. There is an increasing focus on
interconnectivity, the ability to interact with other software and systems, and real time data aggregation.
Electronic medical records and patient health records continue to grow.
Customer and payer consolidation. Our customers and payers, including physicians, health insurance plans,
employers, pharmaceutical companies and others, have been consolidating. We expect that this trend will
continue. Consolidation is increasing customer and payer bargaining power, enhancing purchasing sophistication
and encouraging internalization of testing.
Highly competitive. The clinical testing industry remains fragmented, is highly competitive and is subject to
new competition. Competition is growing from non-traditional competitors. New market entrants with extensive
resources may make acquisitions or expand into our traditional areas of operations. We also are expanding into
new diagnostic testing areas that are highly competitive.
Legislative, regulatory and policy environment. Government oversight of and attention to the healthcare
industry in the United States is significant and increasing. The 2009 American Recovery and Reinvestment Act
included laws designed to expedite the implementation of electronic health records and build a national electronic
health infrastructure in the United States. In addition, there has been extensive discussion of U.S. federal
legislation to reform healthcare. It is not possible to predict whether U.S. federal legislation to reform healthcare
will be enacted, or the nature or impact of any such legislation.
Prevention and wellness. There is an increased awareness of the benefits of, and increased interest in,
preventative medicine and wellness. Consumers, employers, health plans and government agencies increasingly
are focusing on helping the healthy stay healthy, detecting symptoms among those at risk and providing
preventative care that helps avoid disease.
Globalization. There is a growing demand for healthcare services in emerging market countries.
Opportunities are arising to participate in the restructuring or growth of the healthcare systems in these countries.
Additionally, our customers are establishing positions outside the United States. Demographic changes globally
may also create opportunities.
Customers and Payers. We provide testing services to a broad range of customers, with orders for clinical
testing generally generated by physicians, hospitals and employers. In most cases, the customer that orders the
testing is not responsible for the payments for services. We consider a party that refers a test to us a “customer”
and a party that reimburses us a “payer.” Depending on the billing arrangement and applicable law, the payer
may be (1) a third party responsible for providing health insurance coverage to patients, such as a health
insurance plan, self-insured employer benefit fund, or the traditional Medicare or Medicaid program, (2) the
patient or (3) the physician or other party (such as a hospital, another laboratory or an employer) who referred
the testing to us.
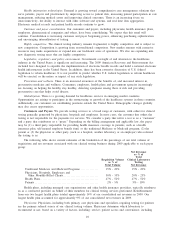
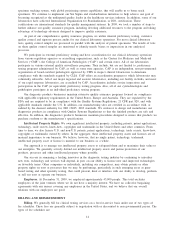
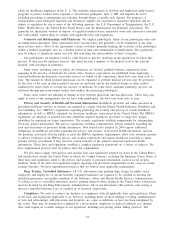
The following table shows current estimates of the breakdown of the percentage of our total volume of
requisitions and net revenues associated with our clinical testing business during 2009 applicable to each payer
group:
Requisition Volume
as % of
Total Volume
Net Revenues
as % of
Total
Clinical Laboratory
Testing
Net Revenues
Traditional Medicare and Medicaid Programs .............. 15% - 20% 15% - 20%
Physicians, Hospitals, Employers and
Other Monthly-Billed Clients. ........................... 30% - 35% 20% - 25%
Health Plans.............................................. 47% - 52% 47% - 52%
Patients .................................................. 2% - 5% 5% - 10%
Health plans, including managed care organizations and other health insurance providers, typically reimburse
us as a contracted provider on behalf of their members for clinical testing services performed. Reimbursement
from our two largest health plans totaled approximately 14% of our consolidated net revenues in 2009. Our
largest health plan accounted for approximately 9% of our consolidated net revenues in 2009.
Physicians. Physicians, including both primary care physicians and specialists, requiring testing for patients
are the primary referral source of our clinical testing volume. Physicians determine which laboratory to
recommend or use, based on a variety of factors, including: service; patient access and convenience, including
10