CVS 2009 Annual Report Download - page 18
Download and view the complete annual report
Please find page 18 of the 2009 CVS annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
Before the 2007 merger that transformed CVS and Caremark
into the nation’s largest pharmacy health care provider,
Caremark had long established itself as a leading PBM. Its
core strengths included generic substitution, mail service,
network management, specialty pharmacy, disease
management, and other clinical programs.
A VARIETY OF UNIQUE, VALUE-ADDED SERVICES
Today’s CVS Caremark plan members still enjoy all of
these traditional offerings, with access to an even larger
network of more than 64,000 retail pharmacies. In
addition, we now offer a variety of unique, value-added
services at our approximately 7,000 CVS/pharmacy loca-
tions, our mail and specialty pharmacies, our MinuteClinics,
call centers, and proprietary websites. All these services
are designed with a common goal: to lower costs while
improving the plan member experience. We are keenly
focused on achieving channel optimization, greater
adherence to prescription drug therapies, higher generic
drug utilization, appropriate use of specialty drugs, and
better health outcomes.
Through our First Fill Counseling program – aimed
at plan members with common chronic conditions –
our in-store CVS pharmacists counsel patients on the
importance of staying on prescribed medications. This
face-to-face engagement has resulted in a 15 percent
improvement in adherence.
Plan designs that promote the use of voluntary, 90-day
maintenance prescriptions help lower costs for health
plans, plan sponsors, and their members. Through
Maintenance Choice, we do this more effectively than
other PBMs by letting eligible plan members choose the
channel that works best for them – mail or pickup at a
conveniently located CVS/pharmacy. Moreover, under
Maintenance Choice key performance measures, such as
adherence to therapy, formulary compliance, and generic
substitution rate, are as good as or better than those of
traditional mandatory mail plan designs.
Some patients who receive their 90-day prescriptions by
mail renew too late to avoid a gap in their drug therapies.
We’ve solved this problem with our Bridge Supply offering.
Eligible plan members can simply stop by their local
CVS/pharmacy, and we’ll provide the medication they
need until their new 90-day supply arrives.
Our integrated offerings don’t end there. At many of
our approximately 570 MinuteClinics across 56 markets,
we’ve launched pilot programs that allow us to provide
health screenings, injection training, and other services
to plan members.
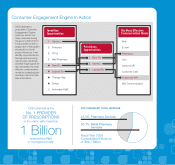
PROVIDING A SINGLE VIEW OF THE PATIENT
Another unique tool that will help broaden our clinical
programs across our asset base is the Consumer Engage-
ment Engine, or CEE. It will provide us with a single
view of the patient across all our touch points – from our
retail and specialty pharmacies to our mail order centers,
MinuteClinics, and websites. The CEE is powered by
clinical rules that will help identify opportunities for
improved health outcomes and cost savings, providing
our pharmacists with easy, actionable messaging for
counseling patients. Implemented first in our PBM
customer care center in the fourth quarter of 2009, the
CEE will go live at all retail locations in 2010. For many
Caremark plan members, their interactions with our
pharmacists across the enterprise should be richer and
more helpful than ever, and we expect to deliver even
better clinical and financial results for our clients.
The Consumer Engagement Engine is powered by clinical rules that will help
identify opportunities for improved health outcomes and cost savings.
“”
We provide more value-added services than any standalone PBM
or retail pharmacy can on its own.
CVS Caremark
14