CVS 2009 Annual Report Download - page 10
Download and view the complete annual report
Please find page 10 of the 2009 CVS annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
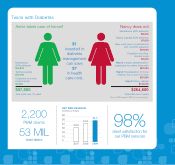
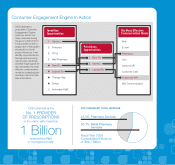
Health plans and plan sponsors choose a pharmacy
benefits manager for its ability to improve savings as well
as the plan member experience. These are challenging
goals in an environment of ever-rising health care costs,
yet CVS Caremark excels at both for our 2,200 clients and
53 million plan members. Our capabilities extend across
the entire PBM spectrum, from mail order and specialty
pharmacies to extensive clinical programs, unique retail
options, and our innovative plan designs.
CLINICAL PROGRAMS THAT PROMOTE ADHERENCE
Research has shown that the failure of patients to adhere
to their prescription medications costs the health care
system $290 billion annually. So, in addition to tiered
formularies and other aspects of plan design that help
control prescription costs, we continue to focus on clinical
programs that promote compliance, adherence, and
improved disease management.
Our Accordant® programs treat 16 rare chronic conditions,
including cystic fibrosis, hemophilia, and multiple sclerosis.
Accordant also treats 11 common chronic conditions such
as adult asthma, congestive heart failure, and diabetes,
and those programs are now managed through our alliance
with Inverness Medical Innovations and its Alere L.L.C.
health management business. Alere is a leader in health
services for wellness, disease management, oncology,
and complex case management. Through Alere, we’ve
been able to expand our clinical offerings to include,
among other things, programs tailored to meet the needs
of women and children.
UNIQUELY POSITIONED TO CONTROL SPECIALTY
PHARMACY COSTS
CVS Caremark is the leading player in the specialty
pharmacy sector, generating approximately $10 billion
in specialty pharmacy sales in 2009. Specialty patients
comprise 1 percent of the population, yet they account
for 33 percent of the total amount spent on health care.
We’re uniquely positioned to help our PBM clients control
specialty spending. For example, our Specialty Guideline
Management program helps identify inappropriate
utilization, in some cases reducing a client’s specialty
spend by more than 5 percent in a given year. Like other
PBMs, we operate specialty mail facilities, but unlike our
competitors, we also own 49 CarePlus™ specialty stores
where patients can benefit from face-to-face counseling
with highly trained pharmacists. Some of our plans offer
the added option of specialty pickup at CVS/pharmacy
locations. Through MinuteClinic, we’ve also launched
pilot programs where our practitioners can teach specialty
patients the proper way to inject their medications.
With our investment in Generation Health, Inc., we’re
accelerating our commitment to personalized medicine
and will make genomic benefit management an integral
part of our PBM offering. If we can identify how an
individual’s genetic variations are likely to impact his or
her response to a particular treatment, we can improve
outcomes and reduce drug spending dramatically.
Approximately 1,700 such tests exist today, with at least
100 more being added annually. Incorporating this offering
is just one more way in which CVS Caremark continues
to raise the bar for PBMs.
Our Specialty Guideline Management program helps identify
inappropriate utilization, in some cases reducing a client’s
specialty spend by more than 5 percent in a given year.
“”
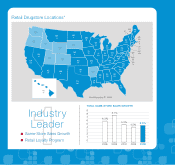
We are a world-class PBM with an impressive track record of improving
savings for health plans, plan sponsors, and their members.
CVS Caremark
6