Quest Diagnostics 2010 Annual Report Download - page 47
Download and view the complete annual report
Please find page 47 of the 2010 Quest Diagnostics annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Healthcare Reform
In March 2010, U.S. federal legislation was enacted which is likely to have a significant impact on, among
other things, access to and the cost of healthcare in the United States. The legislation provides for extensive
health insurance reforms and expands coverage for approximately 32 million previously uninsured Americans,
which will result in expanded access to healthcare. In addition, the legislation eliminates patient cost-sharing for
certain prevention and wellness benefits for health insurance plans that are not “grandfathered.” We believe these
changes will benefit our industry by leading to increased utilization of our services.
These benefits are expected to be partially offset by provisions of the legislation aimed at reducing the
overall cost of healthcare. Impacting laboratories specifically, the legislation provides for annual reductions in the
Medicare clinical laboratory fee schedule of 1.75% for five years beginning in 2011 and includes a productivity
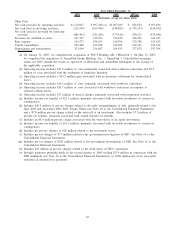
adjustment which reduces the CPI market basket update beginning in 2011. In 2010, approximately 12% of our
consolidated revenues were reimbursed by Medicare under the clinical laboratory fee schedule. The legislation
also imposes an excise tax on the seller for the sale of certain medical devices in the United States, including
those purchased and used by laboratories, beginning in 2013.
In addition, the legislation is focused on reducing the growth of healthcare costs. The legislation establishes
the Independent Payment Advisory Board, which will be responsible, beginning in 2014, annually to submit
proposals aimed at reducing Medicare cost growth while preserving quality. These proposals automatically will be
implemented unless Congress enacts alternative proposals that achieve the same savings targets. Further, the
legislation calls for a Center for Medicare and Medicaid Innovation that will examine alternative payment
methodologies and conduct demonstration programs.
We believe that the legislation will be a net positive for our industry over the long term due to expanded
coverage and the elimination of patient cost-sharing for certain prevention and wellness benefits, and that we are
well positioned to respond to the evolving healthcare environment and related market forces; however, our failure
to adapt to these changes could be detrimental to our business.
Reimbursement for Services
Payments for clinical testing services are made by physicians, hospitals, employers, healthcare insurers,
patients and the government. Physicians, hospitals and employers are typically billed on a fee-for-service basis
based on negotiated fee schedules. Fees billed to healthcare insurers and patients are based on the laboratory’s
patient fee schedule, subject to any limitations on fees negotiated with the healthcare insurers or with physicians
on behalf of their patients. Medicare and Medicaid reimbursements are based on fee schedules set by
governmental authorities.
Government payers, such as Medicare and Medicaid, as well as healthcare insurers and larger employers,
have taken steps and may continue to take steps to control the cost, utilization and delivery of healthcare
services, including clinical testing services. In December 2010, Congress delayed by one year a potential 30%
decrease in the Medicare fee schedule for pathology and other physician services performed for patients and
billed under Part B of the Medicare program. In 2010, approximately 3% of our consolidated revenues were
reimbursed based on this fee schedule.
Healthcare insurers, which typically negotiate directly or indirectly on behalf of their members, represent
approximately one-half of our clinical testing volumes and one-half of our net revenues from our clinical testing
business. Larger healthcare insurers typically contract with large commercial clinical laboratories because they can
provide services to their members on a national or regional basis. In addition, larger commercial clinical
laboratories are better able to achieve the low-cost structures necessary to profitably service the members of large
healthcare insurers and can provide test utilization data across various products in a consistent format. In certain
markets, such as California, healthcare insurers may delegate their covered members to independent physician
associations, which in turn negotiate with laboratories for clinical testing services on behalf of their members.
The trend of consolidation among physicians, hospitals, employers, healthcare insurers and other
intermediaries has continued, resulting in fewer but larger customers and payers with significant bargaining power
to negotiate fee arrangements with healthcare providers, including clinical laboratories. Healthcare insurers often
require that clinical testing service providers accept discounted fee structures or assume all or a portion of the
utilization risk associated with providing testing services to their members enrolled in highly-restricted plans
through capitated payment arrangements. Under these capitated payment arrangements, we and the healthcare
insurers agree to a predetermined monthly reimbursement rate for each member enrolled in a restricted plan,
generally regardless of the number or cost of services provided by us. Our cost to perform testing services
reimbursed under capitated payment arrangements is not materially different from our cost to perform testing
44