CVS 2014 Annual Report Download - page 18
Download and view the complete annual report
Please find page 18 of the 2014 CVS annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
on early extinguishment of debt in 2014 and the gain
from a legal settlement in 2013). And we achieved this
strong growth even after forgoing approximately 8 cents
in earnings per share from exiting the tobacco category.
We’ve benefited from a number of growth drivers,
especially our ability to increase enterprise share of
prescriptions dispensed through our many channels.
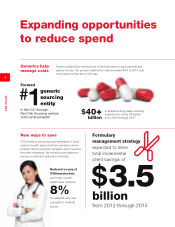
We also filled more than 80 percent of prescriptions
using generic equivalents, which are more cost effective
for patients and payors and are more profitable for
us than branded drugs. Looking ahead, more than
$40 billion of branded drugs are expected to lose
patent protection and effectively be replaced by generic
equivalents between 2015 and 2017. Furthermore,
we completed the formation of our Red Oak Sourcing
venture with Cardinal Health to create the largest generic
sourcing entity in the United States. Our combined
scale, along with our knowledge and expertise, should
lead to even greater savings for our clients, their
members, and CVS Health.
We generated $6.5 billion in free cash flow in 2014 and
once again returned more than $5 billion to shareholders
through dividends and share repurchases. Our board of
directors increased our quarterly dividend by 22 percent
last year and recently approved a 27 percent increase
for 2015. That marks our 12th consecutive year of
increases and keeps us solidly on track toward our
dividend payout ratio target of 35 percent by 2018.
With our December 2014 announcement of a new
$10 billion share repurchase program, we began 2015
with approximately $12.7 billion available to repurchase
CVS Health shares when we identify favorable oppor-
tunities. More than $7 billion is expected to be returned
to our shareholders through dividends and share
repurchases in 2015.
CVS Health shares produced a total return of 36.6 per-
cent in 2014. Over the same period, the S&P 500
Index and the Dow Jones Industrial Average returned
13.7 percent and 10.0 percent, respectively. We have
outperformed these indices on a three-, five-, and
10-year basis as well. Our 2014 stock performance
also outpaced the 25.3 percent return of the S&P 500
Health Care Index.
Our core strengths and integrated offerings drove
another successful PBM selling season
Our CVS/caremark PBM offers competitive pricing, high
levels of service and execution, and unmatched services
that continue to resonate with payors. As a result, 2014
revenues increased by 16 percent to $88 billion in our
Pharmacy Services segment. After a successful selling
season, we started 2015 with $7.0 billion in gross new
business spread among health plans, government
payors, and employers. With a 96 percent retention rate,
net new business for 2015 totaled $3.6 billion.
Clients value the strength of CVS/caremark’s adherence
programs, specialty services, and advanced formulary
strategies. Pharmacy Advisor, Maintenance Choice,
Specialty Connect, and our other integrated offerings
have played an increasingly important role in our ability to
win and retain business. At present, no other PBM can
offer these differentiated services and capabilities.
Pharmacy Advisor, our industry-leading clinical program
for plan members with chronic diseases, currently
addresses diabetes, cardiovascular conditions, and
eight other disease states. Now available to our
Medicare and Medicaid plans as well, it is helping them
improve the clinical star measures that impact their
reimbursement rates.
With more than 20 million plan members enrolled in
Maintenance Choice in 2015, growth in participation has
exceeded 85 percent in just three years. We are also
seeing growing interest in our new Specialty Connect
delivery option. Similar to Maintenance Choice, it offers
specialty patients the flexibility to receive their prescrip-
tions by mail or at one of our stores.
CVS/caremark’s retail network claims have risen
significantly over the past six years, from about 575 mil-
lion to 930 million prescriptions. Over the same period,
CVS/pharmacy’s share of the CVS/caremark book of
business has grown from 19 percent to approximately
31 percent. We are gaining a growing share of a
growing business, highlighting the success of our chan-
nel-agnostic approach and the power of our integrated
business model.
PBM clients are also increasingly incorporating
CVS/minuteclinic services into their plans, improving
member access to health care while lowering overall
costs. For example, our pilot plan to reduce or eliminate
co-payments for plan members now covers 1.2 million
lives. That’s up from 88,000 in 2012.
We are reinventing specialty with a unique suite
of assets to address rising costs
Our specialty pharmacy business continues to grow
rapidly, with revenues from the specialty drugs we
dispensed and managed across the enterprise totaling
$31 billion in 2014. The overall specialty market is
projected to reach $235 billion and 50 percent of total
drug spend by 2018—compared with just 38 percent
this past year—as utilization of costly new therapies
16
CVS Health