CVS 2007 Annual Report Download - page 12
Download and view the complete annual report
Please find page 12 of the 2007 CVS annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.8 I CVS Caremark
“ In the short time since completing our merger, we’ve made substantial
progress in integrating our two companies. We brought PharmaCare,
CVS’ legacy PBM business, under the Caremark umbrella, connected all
our back-end systems, and are set to achieve more than $700 million in
cost-saving synergies in 2008. That’s over 50 percent higher than our
original target at the time we rst announced the merger.”
$700 million in cost-saving syner-
gies in 2008. That’s over 50 percent
higher than our original target at the
time we first announced the merger.
We’ve also made important progress
in developing differentiated offerings
that we believe will lead to enhanced
growth for our company over time.
Obviously, we’re offering payors and
patients all the services they would
expect from a world-class PBM;
however, we plan to take those
services a step further.
For example, let’s take the area
of compliance. One of the simplest
ways for a PBM to control payor
costs and improve outcomes is
by encouraging patients to take the
medicine prescribed to them and to
renew their prescriptions promptly.
Any PBM has the capability to do
this by contacting these patients
over the telephone or by mail.
However, face-to-face interaction
is far more effective, and our
CVS/pharmacy stores give us the
unique capability to get closer to
the consumer. We’re developing
programs that tap into the com-
bined 23,000 pharmacists and
MinuteClinic practitioners in our
locations across the country.
We also intend to build upon our
No. 1 position in the high-growth
specialty pharmacy market, lever-
age our ExtraCare card and all its
unique benefits among our millions
of covered lives, enhance our health
management programs, and increase
use of MinuteClinic by our PBM
clients. We’ll implement some of
our initiatives relatively quickly;
others will happen over time.
We’re leveraging opportunities for
greater protability in the pharmacy.
In both our retail and mail order
pharmacies, we are benefiting from
the aging population, greater utiliza-
tion among seniors due to Medicare
Part D, and the increasing use of
generic drugs. Although their lower
prices depress revenue growth
and we continue to see pressure
on pharmacy reimbursement rates,
generics are more profitable than
brand name drugs and help drive
margin expansion. Moreover,
CVS Caremark is now the largest
purchaser of generic drugs in
the United States, which enables
us to drive down costs.
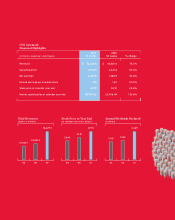
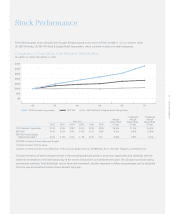
In 2007, the company had a
63 percent generic dispensing
rate at retail. With approximately
$70 billion in branded drug sales
coming off patent in the next
five years, we expect that figure
to rise to 75 percent by 2012.
We should see similar gains for
Caremark’s PBM business, whose
generic dispensing rate is currently
at 60 percent.