CVS 2006 Annual Report Download - page 38
Download and view the complete annual report
Please find page 38 of the 2006 CVS annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
2006 Annual Report 35
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
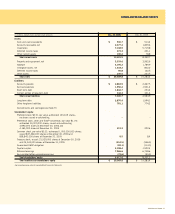
Property and Equipment
Property, equipment and improvements to leased premises are depreciated
using the straight-line method over the estimated useful lives of the assets,
or when applicable, the term of the lease, whichever is shorter. Estimated
useful lives generally range from 10 to 40 years for buildings, building
improvements and leasehold improvements and 5 to 10 years for fixtures
and equipment. Repair and maintenance costs are charged directly to
expense as incurred. Major renewals or replacements that substantially
extend the useful life of an asset are capitalized and depreciated.
Following are the components of property and equipment included in
the consolidated balance sheets as of the respective balance sheet dates:
Dec. 30, Dec. 31,
In millions 2006 2005
Land $ 601.3 $ 322.4
Building and improvements 801.9 631.0
Fixtures and equipment 4,347.4 3,484.1
Leasehold improvements 1,828.5 1,496.7
Capitalized software 219.1 198.6
Capital leases 229.3 1.3
8,027.5 6,134.1
Accumulated depreciation
and amortization (2,693.9) (2,181.5)
$ 5,333.6 $ 3,952.6
The Company capitalizes application development stage costs for significant
internally developed software projects. These costs are amortized over a
five-year period. Unamortized costs were $75.5 million as of December 30,
2006 and $84.3 million as of December 31, 2005.
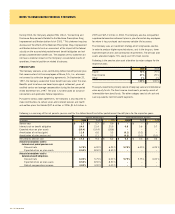
Impairment of Long-Lived Assets
The Company accounts for the impairment of long-lived assets in accordance
with SFAS No. 144, “Accounting for Impairment or Disposal of Long-Lived
Assets.” As such, the Company groups and evaluates fixed and finite-lived
intangible assets excluding goodwill, for impairment at the individual store
level, which is the lowest level at which individual cash flows can be
identified. When evaluating assets for potential impairment, the Company
first compares the carrying amount of the asset group to the individual
store’s estimated future cash flows (undiscounted and without interest
charges). If the estimated future cash flows used in this analysis are less
than the carrying amount of the asset group, an impairment loss calculation
is prepared. The impairment loss calculation compares the carrying
amount of the asset group to the individual store’s estimated fair value
based on estimated future cash flows (discounted and with interest
charges). If the carrying amount exceeds the individual store’s estimated
future cash flows (discounted and with interest charges), the loss is
allocated to the long-lived assets of the group on a pro rata basis using
the relative carrying amounts of those assets.
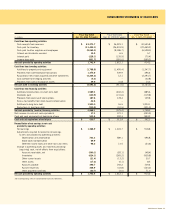
Revenue Recognition
For all sales other than third party pharmacy sales, the Company
recognizes revenue from the sale of merchandise at the point of sale.
For third party pharmacy sales, revenue is recognized at the time the
prescription is filled, which is or approximates when the customer picks
up the prescription. Customer returns are immaterial. Service revenue
from the Company’s pharmacy benefit management segment, which is
recognized using the net method under Emerging Issues Task Force (“EITF”)
Issue No. 99-19, “Reporting Revenue Gross as a Principal Versus Net
as an Agent,” is recognized at the time the service is provided. Service
revenue totaled $194.5 million in 2006, $201.8 million in 2005 and
$129.3 million in 2004.
Premium revenue from the Company’s pharmacy benefit management
segment is accounted for under SFAS No. 113, “Accounting and
Reporting for Reinsurance of Short-Duration and Long-Duration Contracts,”
and is recognized over the period of the contract in proportion to the
amount of insurance coverage provided. Premiums collected in advance
are deferred. Premium revenue totaled $380.1 million in 2006 and
$91.6 million in 2005. There was no premium revenue in 2004.
Insurance
The Company is self-insured for certain losses related to general liability,
workers’ compensation and automobile liability. The Company obtains
third party insurance coverage to limit exposure from these claims. The
Company is also self-insured for certain losses related to health and
medical liabilities.
The Company’s self-insurance accruals, which include reported claims
and claims incurred but not reported, are calculated using standard
insurance industry actuarial assumptions and the Company’s historical
claims experience. During 2005, PharmaCare entered into certain risk-
based or reinsurance arrangements in connection with providing pharmacy
plan management services. Policies and contract claims include actual
claims reported but not paid and estimates of healthcare services
incurred but not reported. The estimated claims incurred but not
reported are calculated using standard insurance industry actuarial
assumptions based on historical data, current enrollment, health service
utilization statistics and other related information and are provided by
third party actuaries.
Vendor Allowances
The Company accounts for vendor allowances under the guidance provided
by EITF Issue No. 02-16, “Accounting by a Customer (Including a Reseller)
for Certain Consideration Received from a Vendor,” and EITF Issue
No. 03-10, “Application of EITF Issue No. 02-16 by Resellers to Sales
Incentives Offered to Consumers by Manufacturers.” Vendor allowances
reduce the carrying cost of inventory unless they are specifically identified
as a reimbursement for promotional programs and/or other services