Cigna 2012 Annual Report Download - page 96
Download and view the complete annual report
Please find page 96 of the 2012 Cigna annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.PART II
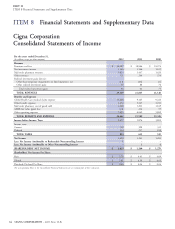
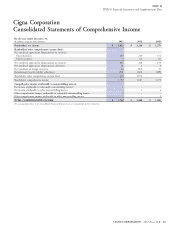
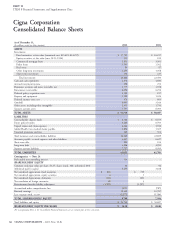
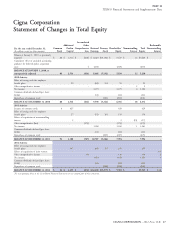
ITEM 8 Financial Statements and Supplementary Data
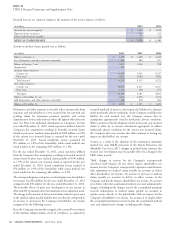
annuity business include adjustments for investment returns statutory disability or other group disability benefit plans. For awards
consistent with requirements of GAAP when a premium deficiency of such offsets that have not been finalized, the Company estimates
exists. the probability and amount of the offset based on the Company’s
experience over the past three to five years.
Certain reinsurance contracts contain GMDB under variable
annuities issued by other insurance companies. These obligations The Company discounts certain claim liabilities related to group
represent the guaranteed death benefit in excess of the contractholder’s long-term disability and workers’ compensation because benefit
account values (based on underlying equity and bond mutual fund payments may be made over extended periods. Discount rate
investments). These obligations are estimated based on assumptions assumptions are based on projected investment returns for the asset
regarding lapse, partial surrenders, mortality, interest rates (mean portfolios that support these liabilities and range from 1.83% to
investment performance and discount rate), market volatility as well 6.25%. When estimates change, the Company records the adjustment
as investment returns and premiums, consistent with the in benefits and expenses in the period in which the change in estimate
requirements of GAAP when a premium deficiency exists. Lapse, is identified. Discounted liabilities associated with the long-term
partial surrenders, mortality, interest rates and volatility are based on disability and certain workers’ compensation businesses were
management’s judgment considering the Company’s experience and $3.2 billion at December 31, 2012 and 2011.
future expectations. The results of futures and swap contracts used in
the GMDB equity and growth interest rate hedge programs are
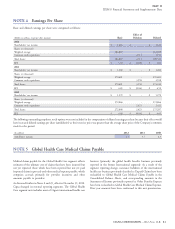
N. Global Health Care Medical Claims
reflected in the liability calculation as a component of investment
Payable
returns. See also Note 7 for additional information.
Medical claims payable for the Global Health Care segment include
both reported claims and estimates for losses incurred but not yet
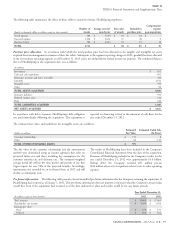
M. Unpaid Claims and Claims Expenses
reported including amounts owed for services from providers and
Liabilities for unpaid claims and claim expenses are estimates of under risk-sharing and quality management arrangements with
payments to be made under insurance coverages (primarily long-term providers. The Company develops estimates for Global Health Care
disability, workers’ compensation and life and health) for reported medical claims payable using actuarial principles and assumptions
claims and for losses incurred but not yet reported. consistently applied each reporting period, and recognizes the
actuarial best estimate of the ultimate liability within a level of
The Company develops these estimates for losses incurred but not yet
confidence, as required by actuarial standards of practice, which
reported using actuarial principles and assumptions based on
require that the liabilities be adequate under moderately adverse
historical and projected claim incidence patterns, claim size,
conditions.
subrogation recoveries and the length of time over which payments are
expected to be made. The Company consistently applies these The liability is primarily calculated using ‘‘completion factors’’ (a
actuarial principles and assumptions each reporting period, with measure of the time to process claims), which are developed by
consideration given to the variability of these factors, and recognizes comparing the date claims were incurred, generally the date services
the actuarial best estimate of the ultimate liability within a level of were provided, to the date claims were paid. The Company uses
confidence, as required by actuarial standards of practice, that require historical completion factors combined with an analysis of current
the liabilities to be adequate under moderately adverse conditions. trends and operational factors to develop current estimates of
completion factors. The Company estimates the liability for claims
The Company’s estimate of the liability for disability claims reported
incurred in each month by applying the current estimates of
but not yet paid is primarily calculated as the present value of expected
completion factors to the current paid claims data. This approach
benefit payments to be made over the estimated time period that a
implicitly assumes that historical completion rates will be a useful
policyholder remains disabled. The Company estimates the expected
indicator for the current period. It is possible that the actual
time period that a policyholder may be disabled by analyzing the rate
completion rates for the current period will develop differently from
at which an open claim is expected to close (claim resolution rate).
historical patterns, which could have a material impact on the
Claim resolution rates may vary based upon the length of time a
Company’s medical claims payable and shareholders’ net income.
policyholder is disabled, the covered benefit period, cause of disability,
benefit design and the policyholder’s age, gender and income level. Completion factors are impacted by several key items including
The Company uses historical resolution rates combined with an changes in: 1) electronic (auto-adjudication) versus manual claim
analysis of current trends and operational factors to develop current processing, 2) provider claims submission rates, 3) membership and
estimates of resolution rates. The reserve for the gross monthly 4) the mix of products. As noted, the Company uses historical
disability benefits due to a policyholder is reduced (offset) by the completion factors combined with an analysis of current trends and
income that the policyholder receives under other benefit programs, operational factors to develop current estimates of completion factors.
such as Social Security Disability Income, workers’ compensation,
74 CIGNA CORPORATION - 2012 Form 10-K