United Healthcare 2009 Annual Report Download - page 42
Download and view the complete annual report
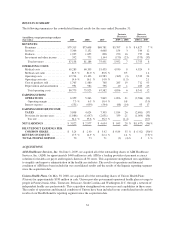
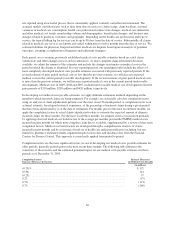
Please find page 42 of the 2009 United Healthcare annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Reporting Segments
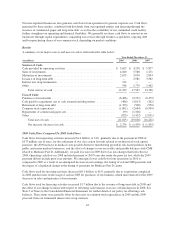
Health Benefits
The revenue growth in Health Benefits for 2008 was primarily due to growth in the number of individuals served
by our Public and Senior Markets Group, premium rate increases for medical cost inflation and the 2008
acquisitions of Sierra, Fiserv Health, and Unison, partially offset by an organic decline in individuals served
through commercial risk-based products and Medicare Part D products and a decrease in investment income.
UnitedHealthcare revenues of $41.8 billion in 2008 increased over the comparable 2007 period by $1.6 billion, or
4%. The UnitedHealthcare increase was primarily driven by the same factors as discussed for Health Benefits in
2008. Ovations revenues of $28.1 billion in 2008 increased over the comparable 2007 period by $1.6 billion, or
6%. The increase was primarily due to an increase in individuals served with the standardized Medicare
Supplement and Medicare Advantage products gained through both organic growth and the Sierra acquisition
and premium rate increases, which were partially offset by a net organic decrease of 675,000 stand-alone
Medicare Part D members primarily due to the reassignment by CMS of certain dual-eligible low income
beneficiaries based on annual price bids. AmeriChoice generated revenues of $6.0 billion in 2008, an increase of
$1.5 billion, or 34%, over the comparable 2007 period, primarily due to an increase in the number of individuals
served by Medicaid plans, premium rate increases and the acquisition of Unison in the second quarter of 2008.
The decrease in Health Benefits earnings from operations was primarily due to pressure on enrollment and gross
margins in the UnitedHealthcare risk-based business and pressure on gross margins in Medicare Part D
prescription drug plans, partially offset by acquisitions. The UnitedHealthcare medical care ratio increased to
83.5% in 2008 from 82.6% in 2007. This increase was primarily driven by the effects of a competitive pricing
environment where price increases, net of customer benefit package changes, did not fully match the rise in
medical costs, and an increased mix of national account pharmaceutical benefit business, which typically carries
a higher medical care ratio. Health Benefits’ operating margin was 6.7% for the year ended December 31, 2008,
a decrease from 9.3% in 2007 primarily driven by the factors discussed above.
The number of individuals served with commercial products increased due to acquisitions, which included the
addition of 1,315,000 fee-based members from Fiserv Health and the addition of 310,000 risk-based individuals
gained through the Sierra acquisition. These additions were partially offset by a net decline in individuals served
with commercial products of 805,000, or 3%, from December 31, 2007, primarily due to a decline in individuals
served with commercial risk-based products and the impact of a competitive commercial risk-based pricing
environment. The number of individuals served by Medicare Advantage products at December 31, 2008
increased through the addition of 60,000 seniors from our acquisition of Sierra and organic growth of 95,000
seniors, partially offset by the divestiture of 30,000 individuals in Nevada related to the Sierra acquisition.
Medicaid enrollment grew due to the addition of 320,000 and 60,000 individuals from our Unison and Sierra
acquisitions, respectively, and strong organic growth of 425,000 individuals.
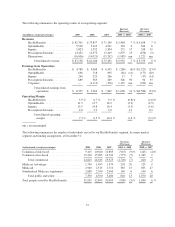
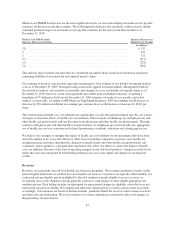
OptumHealth
Increased revenues in OptumHealth were driven by rate increases for medical cost inflation and an increased
number of consumers served by this segment. OptumHealth provided services to approximately 60 million
consumers at December 31, 2008, an increase of approximately 1 million individuals year-over-year.
Earnings from operations and operating margin decreased due to the increased costs for risk-based behavioral
and specialty benefits businesses and the mix of continued growth in lower margin business.
Ingenix
The improvement in Ingenix revenues was due to continued growth in its health intelligence and contract
research businesses as well as from business acquisitions. The decrease in earnings from operations and
operating margin was primarily due to excess staffing costs during 2008 for certain research projects, which were
cancelled, as well as lower demand for certain consulting services due to the current economic environment.
40