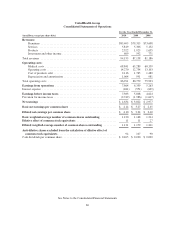
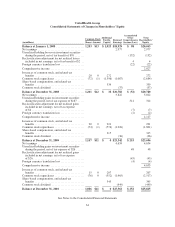
United Healthcare 2010 Annual Report Download - page 66
Download and view the complete annual report
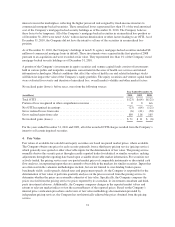
Please find page 66 of the 2010 United Healthcare annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.risk adjustment methodology, CMS calculates the risk adjusted premium payment using diagnosis data from
hospital inpatient, hospital outpatient and physician treatment settings. The Company and health care providers
collect, capture, and submit the necessary and available diagnosis data to CMS within prescribed deadlines. The
Company estimates risk adjustment revenues based upon the diagnosis data submitted and expected to be
submitted to CMS. Risk adjustment data for certain of the Company’s plans is subject to audit by regulators. See
Note 13 of Notes to the Consolidated Financial Statements for additional information regarding these audits.
Service revenues consist primarily of fees derived from services performed for customers that self-insure the
health care costs of their employees and employees’ dependants. Under service fee contracts, the Company
recognizes revenue in the period the related services are performed based upon the fee charged to the customer.
The customers retain the risk of financing health care costs for their employees and employees’ dependants, and
the Company administers the payment of customer funds to physicians and other health care professionals from
customer-funded bank accounts. Since the Company has neither the obligation for funding the health care costs,
nor the primary responsibility for providing the medical care, the Company does not recognize premium revenue
and medical costs for these contracts in its Consolidated Financial Statements.
For both risk-based and fee-based customer arrangements, the Company provides coordination and facilitation of
medical services; transaction processing; customer, consumer and care professional services; and access to
contracted networks of physicians, hospitals and other health care professionals.
Through the Company’s Prescription Solutions pharmacy benefits management (PBM) business, revenues are
derived from products sold through a contracted network of retail pharmacies, and from administrative services,
including claims processing and formulary design and management. Product revenues include ingredient costs
(net of rebates), a negotiated dispensing fee and customer co-payments for drugs dispensed through the
Company’s mail-service pharmacy. In retail pharmacy transactions, revenues recognized always exclude the
member’s applicable co-payment. Product revenues are recognized upon sale or shipment based on contract
terms. Service revenues are recognized when the prescription claim is adjudicated. The Company has entered
into retail service contracts in which it is primarily obligated to pay its network pharmacy providers for benefits
provided to their customers regardless if the Company is paid. The Company is also involved in establishing the
prices charged by retail pharmacies, determining which drugs will be included in formulary listings and selecting
which retail pharmacies will be included in the network offered to plan sponsors’ members. As a result, revenues
are reported on a gross basis. Product revenues also include sales of Ingenix publishing and software products
that are recognized as revenue upon estimated delivery date.
Medical Costs and Medical Costs Payable
Medical costs and medical costs payable include estimates of the Company’s obligations for medical care
services that have been rendered on behalf of insured consumers but for which the Company has either not yet
received or processed claims, and for liabilities for physician, hospital and other medical cost disputes. The
Company develops estimates for medical costs incurred but not reported using an actuarial process that is
consistently applied, centrally controlled and automated. The actuarial models consider factors such as time from
date of service to claim receipt, claim backlogs, care professional contract rate changes, medical care
consumption and other medical cost trends. The Company estimates liabilities for physician, hospital and other
medical cost disputes based upon an analysis of potential outcomes, assuming a combination of litigation and
settlement strategies. Each period, the Company re-examines previously established medical costs payable
estimates based on actual claim submissions and other changes in facts and circumstances. As the liability
estimates recorded in prior periods become more exact, the Company adjusts the amount of the estimates, and
includes the changes in estimates in medical costs in the period in which the change is identified. In every
reporting period, the Company’s operating results include the effects of more completely developed medical
costs payable estimates associated with previously reported periods.
64