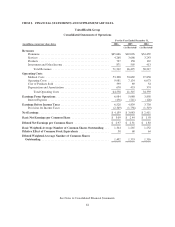
United Healthcare 2006 Annual Report Download - page 70
Download and view the complete annual report
Please find page 70 of the 2006 United Healthcare annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Notes to the Consolidated Financial Statements (As Restated)
1. Description of Business
UnitedHealth Group Incorporated (also referred to as “UnitedHealth Group,” “the Company,” “we,” “us,” and
“our”) is a diversified health and well-being company dedicated to making health care work better. Through
strategically aligned, market-defined businesses, we design products, provide services and apply technologies
that improve access to health and well-being services, simplify the health care experience, promote quality and
make health care more affordable.
2. Summary of Significant Accounting Policies
Basis of Presentation
We have prepared the consolidated financial statements according to accounting principles generally accepted in
the United States of America and have included the accounts of UnitedHealth Group and its subsidiaries. We
have eliminated all intercompany balances and transactions.
Use of Estimates
These consolidated financial statements include certain amounts that are based on our best estimates and
judgments. These estimates require us to apply complex assumptions and judgments, often because we must
make estimates about the effects of matters that are inherently uncertain and will likely change in subsequent
periods. The most significant estimates relate to medical costs, medical costs payable, historic stock option
measurement dates, revenues, intangible asset valuations, asset impairments and contingent liabilities. We adjust
these estimates each period, as more current information becomes available. The impact of any changes in
estimates is included in the determination of earnings in the period in which the estimate is adjusted.
Revenues
Premium revenues are primarily derived from risk-based health insurance arrangements in which the premium is
fixed, typically for a one-year period, and we assume the economic risk of funding our customers’ health care
services and related administrative costs. We recognize premium revenues in the period in which eligible
individuals are entitled to receive health care services. We record health care premium payments we receive from
our customers in advance of the service period as unearned premiums.
Service revenues consist primarily of fees derived from services performed for customers that self-insure the
medical costs of their employees and their dependents. Under service fee contracts, we recognize revenue in the
period the related services are performed based upon the fee charged to the customer. The customers retain the
risk of financing medical benefits for their employees and their employees’ dependents, and we administer the
payment of customer funds to physicians and other health care providers from customer-funded bank accounts.
Because we neither have the obligation for funding the medical expenses, nor do we have responsibility for
delivering the medical care, we do not recognize premium revenue and medical costs for these contracts in our
consolidated financial statements.
For both premium risk-based and fee-based customer arrangements, we provide coordination and facilitation of
medical services; transaction processing; customer, consumer and care provider services; and access to
contracted networks of physicians, hospitals and other health care professionals.
Through our Prescription Solutions pharmacy benefits management (PBM) business, revenues are derived from
products sold through a contracted network of retail pharmacies, and from administrative services, including
claims processing and formulary design and management. Product revenues include ingredient costs net of
rebates, a negotiated dispensing fee and customer co-payments for drugs dispensed through our mail-service
68