United Healthcare 2008 Annual Report Download - page 70
Download and view the complete annual report
Please find page 70 of the 2008 United Healthcare annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.UNITEDHEALTH GROUP
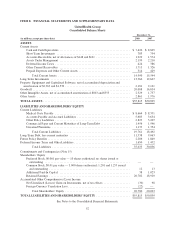
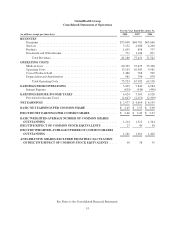
NOTES TO THE CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
of the individual annual out-of-pocket maximum. A settlement is made with CMS based on actual cost
experience, subsequent to the end of the plan year.
•Low-Income Member Cost Sharing Subsidy — For qualifying low-income members, CMS pays on the
member’s behalf some or all of a member’s cost sharing amounts, such as deductibles and coinsurance. The
cost sharing subsidy is funded by CMS through monthly payments to the Company. The Company
administers and pays the subsidized portion of the claims on behalf of CMS, and a settlement payment is
made between CMS and the Company based on actual claims and premium experience, subsequent to the
end of the plan year.
•CMS Risk-Share — Premiums from CMS are subject to risk corridor provisions which compare costs
targeted in the Company’s annual bids to actual prescription drug costs, limited to actual costs that would
have been incurred under the standard coverage as defined by CMS. Variances of more than 5% above or
below the original bid submitted by the Company may result in CMS making additional payments to the
Company or require the Company to refund to CMS a portion of the premiums it received. The Company
estimates and recognizes an adjustment to premium revenues related to the risk corridor payment settlement
based upon pharmacy claims experience. The estimate of the settlement associated with these risk corridor
provisions requires the Company to consider factors that may not be certain, including member eligibility
status differences with CMS. The risk-share adjustment, if any, is recorded as an adjustment to premium
revenues and other current assets or liabilities.
The CMS Premium, the Member Premium, and the Low-Income Premium Subsidy represent payments for the
Company’s insurance risk coverage under the Medicare Part D program and therefore are recorded as Premium
Revenues in the Consolidated Statements of Operations. Premium revenues are recognized ratably over the
period in which eligible individuals are entitled to receive prescription drug benefits. The Company records
premium payments received in advance of the applicable service period in Unearned Premiums in the
Consolidated Balance Sheets.
The Catastrophic Reinsurance Subsidy and the Low-Income Member Cost Sharing Subsidy represent cost
reimbursements under the Medicare Part D program. The Company is fully reimbursed by CMS for costs
incurred for these contract elements and accordingly, there is no insurance risk to the Company. Amounts
received for these subsidies are not reflected as premium revenues, but rather are accounted for as deposits within
Other Policy Liabilities in the Consolidated Balance Sheets. Related cash flows are presented as Customer Funds
Administered within financing activities in the Consolidated Statements of Cash Flows.
As of December 31, 2008, there was a receivable for the Catastrophic Reinsurance Subsidy and the Low-Income
Member Cost Sharing Subsidy of $349 million recorded in Other Current Receivables in the Consolidated
Balance Sheets. As of December 31, 2007, there were amounts on deposit for these subsidies of approximately
$340 million recorded in Other Policy Liabilities in the Consolidated Balance Sheets.
Pharmacy benefit costs and administrative costs under the contract are expensed as incurred and are recognized
in Medical Costs and Operating Costs, respectively, in the Consolidated Statements of Operations.
As a result of the Medicare Part D product benefit design, the Company incurs a disproportionate amount of
pharmacy benefit costs early in the contract year. While the Company is responsible for approximately 67% of a
Medicare Part D beneficiary’s drug costs up to the initial coverage limit, the beneficiary is responsible for 100%
of their drug costs from the initial coverage limit to the out-of-pocket maximum. Consequently, the Company
incurs a disproportionate amount of pharmacy benefit costs in the first half of the contract year as compared with
the last half of the contract year, when comparatively more members will be incurring claims above the initial
60