United Healthcare 2008 Annual Report Download - page 59
Download and view the complete annual report
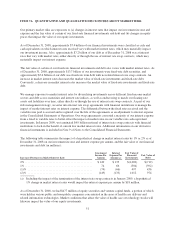
Please find page 59 of the 2008 United Healthcare annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Our estimate of medical costs payable represents management’s best estimate of our liability for unpaid medical
costs as of December 31, 2008, developed using consistently applied actuarial methods. Management believes
the amount of medical costs payable is reasonable and adequate to cover our liability for unpaid claims as of
December 31, 2008, however, actual claim payments may differ from established estimates. Assuming a
hypothetical 1% difference between our December 31, 2008 estimates of medical costs payable and actual
medical costs payable, excluding AARP Medicare Supplement Insurance, 2008 net earnings would increase or
decrease by $48 million and diluted net earnings per common share would increase or decrease by $0.04 per
share.
The current national health care cost inflation rate significantly exceeds the general inflation rate. We use various
strategies to lessen the effects of health care cost inflation. These include setting commercial premiums based on
anticipated health care costs, coordinating care with physicians and other health care professionals and rate
discounts from physicians and other health care professionals. Through contracts with physicians and other
health care professionals, we emphasize preventive health care, appropriate use of health care services consistent
with clinical performance standards, education and closing gaps in care.
We believe our strategies to mitigate the impact of health care cost inflation on our operating results have been
and will continue to be successful. However, other factors including competitive pressures, new health care
and pharmaceutical product introductions, demands from physicians and other health care professionals and
consumers, major epidemics, and applicable regulations may affect our ability to control the impact of health
care cost inflation. Because of the narrow operating margins of our risk-based products, changes in medical cost
trends that were not anticipated in establishing premium rates can create significant changes in our financial
results.
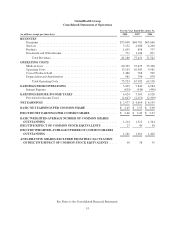
Revenues
Revenues are principally derived from health care insurance premiums. We recognize premium revenues in the
period eligible individuals are entitled to receive health care services. Customers are typically billed monthly at a
contracted rate per eligible person multiplied by the total number of people eligible to receive services, as
recorded in our records. Employer groups generally provide us with changes to their eligible population one
month in arrears. Each billing includes an adjustment for prior period changes in eligibility status that were not
reflected in our previous billing. We estimate and adjust the current period’s revenues and accounts receivable
accordingly. Our estimates are based on historical trends, premiums billed, the level of contract renewal activity
and other relevant information. We revise estimates of revenue adjustments each period and record changes in
the period they become known.
We estimate risk adjustment revenues based upon the diagnosis data submitted and expected to be submitted to
CMS. CMS deploys a risk adjustment model which apportions premiums paid to all health plans according to
health severity and certain demographic factors. The CMS risk adjustment model pays more for members whose
medical history would indicate are expected to have higher medical costs. Under this risk adjustment
methodology, CMS calculates the risk adjusted premium payment using diagnosis data from hospital inpatient,
hospital outpatient and physician treatment settings. Necessary and available diagnosis data collected and
captured by us and health care providers is submitted to CMS within prescribed deadlines.
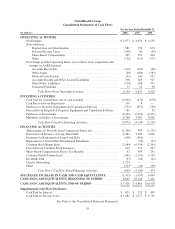
Goodwill, Intangible Assets and Other Long-Lived Assets
As of December 31, 2008, we had long-lived assets, including goodwill, other intangible assets and property,
equipment and capitalized software, of $24.6 billion. We review our goodwill for impairment annually at the
reporting unit level, and we review our remaining long-lived assets for impairment when events and changes in
circumstances indicate we might not recover their carrying value. To determine the fair value of our long-lived
assets and assess their recoverability, we must make assumptions about a wide variety of internal and external
factors including estimated future utility and estimated future cash flows, which in turn are based on estimates of
future revenues, expenses and operating margins. If these estimates or their related assumptions change in the
49