United Healthcare 2007 Annual Report Download - page 63
Download and view the complete annual report
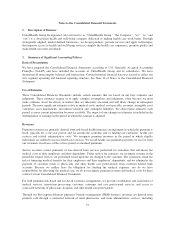
Please find page 63 of the 2007 United Healthcare annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.cost sharing subsidy is funded by CMS through monthly payments to the Company. The Company
administers and pays the subsidized portion of the claims on behalf of CMS, and a settlement payment is
made between CMS and the Company based on actual claims experience, subsequent to the end of the plan
year.
•CMS Risk-Share — If the ultimate per member per month benefit costs of any Medicare Part D regional
plan varies more than 2.5% above or below the level estimated in the original bid submitted by the
Company and approved by CMS, there is a risk-share settlement with CMS subsequent to the end of the
plan year. The risk-share adjustment, if any, is recorded as an adjustment to premium revenues and other
receivables or liabilities.
The CMS Premium, the Member Premium, and the Low-Income Premium Subsidy represent payments for the
Company’s insurance risk coverage under the Medicare Part D program and therefore are recorded as Premium
Revenues in the Consolidated Statements of Operations. Premium revenues are recognized ratably over the
period in which eligible individuals are entitled to receive prescription drug benefits. We record premium
payments received in advance of the applicable service period in Unearned Premiums in the Consolidated
Balance Sheets.
The Catastrophic Reinsurance Subsidy and the Low-Income Member Cost Sharing Subsidy represent cost
reimbursements under the Medicare Part D program. The Company is fully reimbursed by CMS for costs
incurred for these contract elements and, accordingly, there is no insurance risk to the Company. Amounts
received for these subsidies are not reflected as premium revenues, but rather are accounted for as deposits, with
the related liability recorded in Other Policy Liabilities in the Consolidated Balance Sheets. Related cash flows
are presented as Customer Funds Administered within financing cash flows in the Consolidated Statements of
Cash Flows. As of December 31, 2007, the amount on deposit for these subsidies for the 2007 contract year was
approximately $395 million and the payable to CMS for these subsidies for the 2006 contract year was
approximately $55 million.
Pharmacy benefit costs and administrative costs under the contract are expensed as incurred and are recognized
in Medical Costs and Operating Costs, respectively, in the Consolidated Statements of Operations.
As a result of the Medicare Part D product benefit design, the Company incurs a disproportionate amount of
pharmacy benefit costs early in the contract year. While the Company is responsible for approximately 67% of a
Medicare Part D beneficiary’s drug costs up to $2,400, the beneficiary is responsible for 100% of their drug costs
from $2,400 up to $5,451 (at the Company’s discounted purchase price). Consequently, the Company incurs a
disproportionate amount of pharmacy benefit costs in the first half of the contract year as compared with the last
half of the contract year, when comparatively more members will be incurring claims above the $2,400 initial
coverage limit. The uneven timing of Medicare Part D pharmacy benefit claims results in losses in the first half
of the year that entitle the Company to risk-share adjustment payments from CMS. Accordingly, during the
interim periods within the contract year we record a net risk-share receivable from CMS in Other Current Assets
in the Consolidated Balance Sheets and a corresponding retrospective premium adjustment in Premium Revenues
in the Consolidated Statements of Operations. This represents the estimated amount payable by CMS to the
Company under the risk-share contract provisions if the program were terminated based on estimated costs
incurred through that interim period. Those losses are typically expected to reverse in the second half of the year.
The risk-share payable due to CMS for the 2007 contract year through December 31, 2007 was approximately
$145 million. This final risk-share amount is expected to be settled approximately six months after the contract
year-end. The risk-share payable due to CMS as of December 31, 2007 for the 2006 contract year was
approximately $135 million, subject to the reconciliation process with CMS, and was paid in January 2008.
These risk-share payables, totalling $280 million are recorded in Other Policy Liabilities in the Consolidated
Balance Sheets.
Total premium revenues from CMS related to the Medicare Part D program and all other Medicare-related programs
were approximately 25% of our total consolidated revenues for the twelve months ended December 31, 2007.
61