United Healthcare 2007 Annual Report Download - page 22
Download and view the complete annual report
Please find page 22 of the 2007 United Healthcare annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.ITEM 7. MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND
RESULTS OF OPERATIONS
Business Overview
UnitedHealth Group is a diversified health and well-being company, serving approximately 70 million
Americans. Our focus is on enhancing the performance of the health system and improving the overall health and
well-being of the people we serve and their communities. We work with health care professionals and other key
partners to expand access to high quality health care. We help people get the care they need at an affordable cost,
support the physician/patient relationship, and empower people with the information, guidance and tools they
need to make personal health choices and decisions.
Through our diversified family of businesses, we leverage core competencies in advanced technology-based
transactional capabilities; health care data, knowledge and information; and health care resource organization and
care facilitation to make health care work better. We provide individuals with access to quality, cost-effective
health care services and resources. We provide employers and consumers with excellent value, service and
support, and we deliver value to our shareholders by executing a business strategy founded upon a commitment
to balanced growth, profitability and capital discipline.
Management’s Discussion and Analysis of Financial Condition and Results of Operations should be read in
conjunction with our Consolidated Financial Statements and Notes thereto included elsewhere in this Form 10-K.
2007 Financial Performance Highlights
UnitedHealth Group had strong results in 2007. The Company achieved growth across each of its reporting
segments and generated net earnings of $4.7 billion, representing an increase of 12% over 2006. Other financial
performance highlights include:
• Diluted net earnings per common share of $3.42, an increase of 15% over 2006.
• Consolidated revenues of $75.4 billion, an increase of 5% over 2006.
• Earnings from operations of $7.8 billion, up $865 million, or 12%, over 2006.
• Operating margin of 10.4%, up from 9.8% in 2006.
• Cash flows from operations of $5.9 billion, representing 126% of 2007 net earnings.
2007 Results Compared to 2006 Results
Consolidated Financial Results
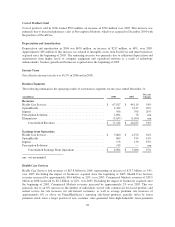
Revenues
Revenues are comprised of premium revenues from risk-based products; service revenues, which primarily
include fees for management, administrative and consulting services; product revenues; and investment and other
income.
Premium revenues are primarily derived from risk-based health insurance arrangements in which the premium is
fixed, typically for a one-year period, and we assume the economic risk of funding our customers’ health care
services and related administrative costs. Service revenues consist primarily of fees derived from services
performed for customers that self-insure the medical costs of their employees and their dependents. For both
premium risk-based and fee-based customer arrangements, we provide coordination and facilitation of medical
services; transaction processing; customer, consumer and care provider services; and access to contracted
networks of physicians, hospitals and other health care professionals. Through our pharmacy benefit management
(PBM) business, Prescription Solutions, revenues are derived from products sold and from administrative
services. Product revenues also include sales of Ingenix syndicated content products.
20