Anthem Blue Cross 2000 Annual Report Download - page 9
Download and view the complete annual report
Please find page 9 of the 2000 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.7
Anthem Insurance Companies, Inc.
Notes to Consolidated Financial Statements (continued)
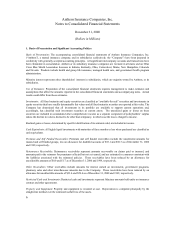
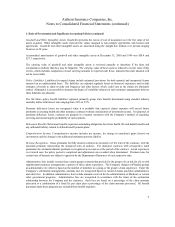
1. Basis of Presentation and Significant Accounting Policies (continued)
Goodwill and Other Intangible Assets: Goodwill represents the excess of cost of acquisition over the fair value of net
assets acquired. Other intangible assets represent the values assigned to non-compete agreements, and licenses and
agreements. Goodwill and other intangible assets are amortized using the straight-line method over periods ranging
from two to 20 years.
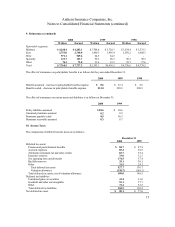
Accumulated amortization of goodwill and other intangible assets at December 31, 2000 and 1999 was $58.4 and
$27.3, respectively.
The carrying value of goodwill and other intangible assets is reviewed annually to determine if the facts and
circumstances indicate that they may be impaired. The carrying value of these assets is reduced to its fair value if this
review, which includes comparison of asset carrying amounts to expected cash flows, indicates that such amounts will
not be recoverable.
Policy Liabilities: Liabilities for unpaid claims include estimated provisions for both reported and unreported claims
incurred on an undiscounted basis. The liabilities are adjusted regularly based on historical experience and include
estimates of trends in claim severity and frequency and other factors, which could vary as the claims are ultimately
settled. Although it is not possible to measure the degree of variability inherent in such estimates, management believes
these liabilities are adequate.
The life future policy benefit liabilities represent primarily group term benefits determined using standard industry
mortality tables with interest rates ranging from 3.0% to 5.5%
Premium deficiency losses are recognized when it is probable that expected claims expenses will exceed future
premiums on existing health and other insurance contracts without consideration of investment income. For purposes of
premium deficiency losses, contracts are grouped in a manner consistent with the Company’ s method of acquiring,
servicing and measuring the profitability of such contracts.
Retirement Benefits: Retirement benefits represent outstanding obligations for retiree health, life and dental benefits and
any unfunded liability related to defined benefit pension plans.
Comprehensive Income: Comprehensive income includes net income, the change in unrealized gains (losses) on
investments and the change in the additional minimum pension liability.
Revenue Recognition: Gross premiums for fully insured contracts are prorated over the term of the contracts, with the
unearned premium representing the unexpired term of policies. For insurance contracts with retrospective rated
premiums, the estimated ultimate premium is recognized as revenue over the period of the contract. Actual experience
is reviewed once the policy period is completed and adjustments are recorded when determined. Premium rates for
certain lines of business are subject to approval by the Department of Insurance of each respective state.
Administrative fees include revenue from certain groups contracts that provide for the group to be at risk for all, or with
supplemental insurance arrangements, a portion of their claims experience. The Company charges self-funded groups
an administrative fee which is based on the number of members in a group or the group’ s claim experience. Under the
Company’ s self-funded arrangements, amounts due are recognized based on incurred claims paid plus administrative
and other fees. In addition, administrative fees include amounts received for the administration of Medicare or certain
other government programs. Administrative fees are recognized in accordance with the terms of the contractual
relationship between the Company and the customer. Such fees are based on a percentage of the claim amounts
processed or a combination of a fixed fee per claim plus a percentage of the claim amounts processed. All benefit
payments under these programs are excluded from benefit expenses.