United Healthcare 2004 Annual Report Download - page 62
Download and view the complete annual report
Please find page 62 of the 2004 United Healthcare annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
60 UNITEDHEALTH GROUP
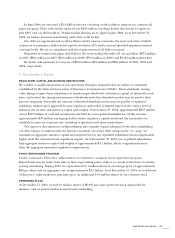
OTHER CONTINGENCIES
In 2002, Oxford, which we acquired on July 29, 2004, entered into agreements with two insurance
companies that guaranteed cost reduction targets related to certain orthopedic medical services. In 2003,
the insurers sought to rescind or terminate the agreements claiming various misrepresentations and
material breaches of the agreements by Oxford. Pursuant to the agreements, Oxford filed claims to
recover approximately $50 million of costs incurred and expensed in excess of the cost reduction targets
for the period from November 2002 to October 2004. An arbitration hearing with the insurance company
holding a large majority of the coverage under the policies was held in January 2005, and a decision was
issued on February 22, 2005, denying the insurer’s ability to rescind or terminate its agreement. As a result
of the decision, Oxford was awarded approximately $30 million in net recoveries. The insurer has not
yet indicated whether it will appeal this decision. Oxford will not record the net recoveries until all
contingencies have been resolved. We believe that the remaining insurer’s claims are also without merit,
and we will vigorously seek to enforce our rights.
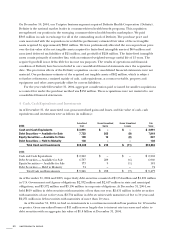
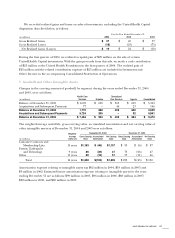
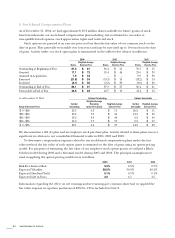
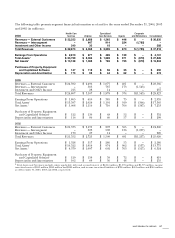
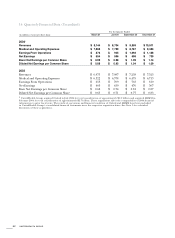
13 Segment Financial Information
Factors used in determining our reportable business segments include the nature of operating activities,
existence of separate senior management teams, and the type of information presented to the company’s
chief operating decision-maker to evaluate our results of operations.
Our accounting policies for business segment operations are the same as those described in the
Summary of Significant Accounting Policies (see Note 2). Transactions between business segments
principally consist of customer service and transaction processing services that Uniprise provides to
Health Care Services, certain product offerings sold to Uniprise and Health Care Services customers
by Specialized Care Services, and sales of medical benefits cost, quality and utilization data and predictive
modeling to Health Care Services and Uniprise by Ingenix. These transactions are recorded at
management’s best estimate of fair value, as if the services were purchased from or sold to third parties.
All intersegment transactions are eliminated in consolidation. Assets and liabilities that are jointly used
are assigned to each segment using estimates of pro-rata usage. Cash and investments are assigned such
that each segment has minimum specified levels of regulatory capital or working capital for non-regulated
businesses. The “Corporate and Eliminations” column also includes eliminations of intersegment
transactions.
Substantially all of our operations are conducted in the United States. In accordance with accounting
principles generally accepted in the United States of America, segments with similar economic
characteristics may be combined. The financial results of UnitedHealthcare, Ovations and AmeriChoice
have been combined in the Health Care Services segment column in the tables presented on the next
page because these businesses have similar economic characteristics and have similar products and
services, types of customers, distribution methods and operational processes, and operate in a similar
regulatory environment, typically within the same legal entity.