United Healthcare 2007 Annual Report Download - page 84
Download and view the complete annual report
Please find page 84 of the 2007 United Healthcare annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.Other Legal Matters
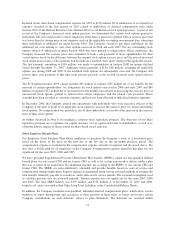
Because of the nature of our businesses, we are routinely made party to a variety of legal actions related to the
design and management of our service offerings. We record liabilities for our estimates of probable costs resulting
from these matters. These matters include, but are not limited to, claims relating to health care benefits coverage,
medical malpractice actions, contract disputes and claims related to disclosure of certain business practices.
Beginning in 1999, a series of class action lawsuits were filed against UnitedHealthcare, PacifiCare, and virtually
all major entities in the health benefits business. These lawsuits were consolidated in a multi-district litigation in
the Southern District Court of Florida. The health care provider plaintiffs alleged statutory violations, including
violations of the Racketeer Influenced Corrupt Organization Act (RICO) in connection with alleged undisclosed
reimbursement policies. Other allegations included breach of state prompt payment laws and breach of contract
claims for failure to timely reimburse health care providers for medical services rendered. The consolidated suits
seek injunctive, compensatory and equitable relief as well as restitution, costs, fees and interest payments. The
trial court granted the health care providers’ motion for class certification. The Eleventh Circuit Court of Appeals
affirmed the class action status of certain of the RICO claims, but reversed as to the breach of contract, unjust
enrichment and prompt payment claims. Most of the co-defendents have settled. On January 31, 2006, the trial
court dismissed all claims against PacifiCare, and on June 19, 2006, the trial court dismissed all claims against
UnitedHealthcare brought by the lead plaintiffs. On June 13, 2007, the Eleventh Circuit Court of Appeals
affirmed those decisions. Included in the multidistrict litigation are tag-along lawsuits which contain claims
against the Company similar to the claims dismissed in the lead case. The tag-along cases were stayed pending
resolution of the lead case. That stay has not been lifted, but it is anticipated that the trial court will now lift the
stay and address the continuing viability of the tag-along claims. The plaintiffs in a number of the tag-along cases
have sought to remand the cases to alternate forums. We have opposed these efforts and have moved the court to
apply its June 2006 summary judgment ruling, and its other applicable pretrial rulings, to those cases. On
February 12, 2008, the court denied all pending motions without prejudice and set a briefing schedule for future
motions, including motions for summary judgment. We are vigorously defending against the remaining claims.
On March 15, 2000, the American Medical Association (AMA) filed a lawsuit against the Company and
affiliated entities, such as UnitedHealthcare, in state court in New York. We removed the case to the United
States District Court for the Southern District of New York. The suit originally alleged causes of action based on
ERISA, as well as breach of contract and the implied covenant of good faith and fair dealing, deceptive acts and
practices, and trade libel in connection with the calculation of reasonable and customary reimbursement rates for
non-network health care providers by the Company’s affiliates. On May 26, 2004, we filed a motion for partial
summary judgment seeking the dismissal of certain claims and parties. On June 15, 2007, the trial court granted
part of our motion for summary judgment. The Court ruled that AMA does not have standing to pursue ERISA
claims for benefits on behalf of their physician members. The Court also ruled that the subscriber plaintiffs (and
physician plaintiffs with valid assignments from subscribers) can only seek monetary damages under ERISA for
those reimbursements that were actually appealed through the health plans’ appeal processes. The Court found
that such appeals are not “futile,” as plaintiffs alleged. Finally, the Court found that the health care providers and
plan participants have no standing to bring a claim where the provider waived its right to collect the balance from
the subscriber. While these decisions narrow the case, they do not resolve the non-ERISA claims or ERISA
breach of fiduciary duty claims. On July 10, 2007, plaintiffs filed a fourth amended complaint adding RICO and
antitrust claims and realleging several of their prior ERISA and state law claims. On September 24, 2007, we
moved to dismiss the RICO and antitrust claims in the fourth amended complaint. On January 11, 2008, the
parties finalized briefing on the motion to dismiss and are awaiting the court’s ruling on the motion. We are
vigorously defending against the remaining claims.
On February 13, 2008, the New York Attorney General (“NYAG”) announced that (1) his office is conducting an
industry-wide investigation into health insurers’ provider reimbursement practices; (2) his office has issued
subpoenas to 16 health insurance companies in connection with such investigation, including one of our
subsidiaries; and (3) his office intends to file suit against UnitedHealth Group and four of our subsidiaries. On
82