Anthem Blue Cross 2010 Annual Report Download - page 14
Download and view the complete annual report
Please find page 14 of the 2010 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
WellPoint works to simplify the connection between Health, Care and Value. We help to
improve the health of our communities, deliver better care to members, and provide greater
value to our customers and shareholders. WellPoint is the nation’s largest health benefits
company in terms of medical enrollment, with more than 33 million members in our affiliated
health plans, and a total of more than 69 million individuals served through our subsidiaries.
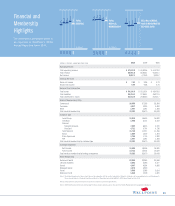
Key
Financial
Metrics:
Customer Base
in Affiliated Plans:
$57.8
Operating Revenue
(dollars in billions)
83.2%
Benefit Expense Ratio
$185*
Claims and Administered Benefits
(dollars in billions)
15.3%
Selling, General and
Administrative Expense Ratio
1 in 9Americans
Individual
Individual customers under age 65 and their covered
dependents.
Local Group
Employer customers with less than 5% of eligible
employees located outside of the headquarter state, as
well as customers with up to 5,000 eligible employees.
National Accounts
Generally multi-state employer groups primarily head-
quartered in a WellPoint service area with at least 5% of
the eligible employees located outside of the headquarter
state and with more than 5,000 eligible employees. Some
exceptions are allowed based on broker relationships.
Senior
Medicare-eligible individual members age 65 and over
who have enrolled in Medicare Advantage, a managed
care alternative for the Medicare program, or who have
purchased Medicare Supplement benefit coverage.
State Sponsored
Eligible members with state-sponsored managed care
alternatives for the Medicaid and State Children’s Health
Insurance programs that we manage.
BlueCard®
BlueCard host members represent enrollees of Blue Cross
and/or Blue Shield plans not owned by WellPoint who
receive health care services in our Blue Plan markets.
Federal Employee Program (FEP)
United States government employees and their depen-
dents within our geographic markets through our
participation in the national contract between the Blue
Cross Blue Shield Association and the U.S. Office of
Personnel Management.
Specialty
Our plans offer Behavioral Health, Life, Disability, Dental
and Vision products which provide administrative
efficiency and enhanced product value.
33.3
Medical Members
WellPoint’s affiliated health
plans have among the most
diverse customer bases in
the industry.
Million
2 0 1 0 S U M M A R Y A N N U A L R E P O R T
12
are covered
by WellPoint’s
affiliated
health plans
WellPoint at a Glance
* Approximate total claims paid for commercial and consumer business, fully insured and self-funded; the Federal Employee Program; and claims administered through our
National Government Services business unit.