United Healthcare 2008 Annual Report Download - page 66
Download and view the complete annual report
Please find page 66 of the 2008 United Healthcare annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.UNITEDHEALTH GROUP
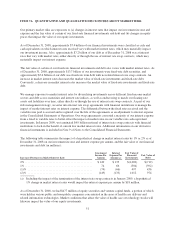
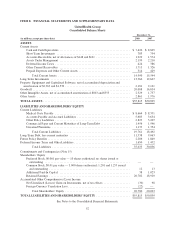
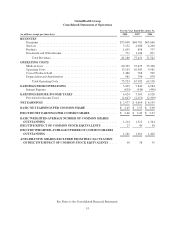
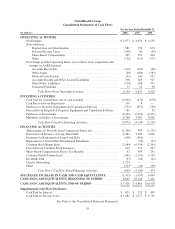
NOTES TO THE CONSOLIDATED FINANCIAL STATEMENTS
1. Description of Business
UnitedHealth Group Incorporated (also referred to as “UnitedHealth Group” and “the Company”) is a diversified
health and well-being company dedicated to making health care work better. The Company emphasizes
enhancing the performance of the health system and improving the overall health and well-being of the people it
serves and their communities. The Company helps people get the care they need at an affordable cost, supports
the physician/patient relationship, and empowers people with the information, guidance and tools they need to
make personal health choices and decisions.
The Company’s primary focus is on improving the health care system by simplifying the administrative
components of health care delivery, promoting evidence-based medicine as the standard for care, and providing
relevant, actionable data that physicians, health care professionals, consumers, employers and other participants
in health care can use to make better, more informed decisions.
Through its diversified family of businesses, the Company leverages core competencies in advanced technology-
based transactional capabilities; health care data, knowledge and information; and health care resource
organization and care facilitation to improve access to health and well-being services, simplify the health care
experience, promote quality and make health care more affordable.
2. Basis of Presentation and Summary of Significant Accounting Policies
Basis of Presentation
The Company has prepared the Consolidated Financial Statements according to U.S. Generally Accepted
Accounting Principles (GAAP) and has included the accounts of UnitedHealth Group and its subsidiaries.
Certain prior year amounts have been reclassified to conform to current year presentation. The Company has
eliminated intercompany balances and transactions.
Use of Estimates
These Consolidated Financial Statements include certain amounts that are based on the Company’s best estimates
and judgments. These estimates require the application of complex assumptions and judgments, often because
they involve matters that are inherently uncertain and will likely change in subsequent periods. The Company’s
most significant estimates relate to medical costs, medical costs payable, revenues, goodwill, other intangible
assets, investments and contingent liabilities. The Company adjusts these estimates each period, as more current
information becomes available. The impact of any changes in estimates is included in the determination of
earnings in the period in which the estimate is adjusted.
Revenues
Premium revenues are primarily derived from risk-based health insurance arrangements in which the premium is
fixed, typically for a one-year period, and the Company assumes the economic risk of funding its customers’
health care services and related administrative costs. The Company recognizes premium revenues in the period in
which eligible individuals are entitled to receive health care services. The Company records health care premium
payments received from its customers in advance of the service period as unearned premiums.
CMS deploys a risk adjustment model which apportions premiums paid to all health plans according to health
severity and certain demographic factors. The CMS risk adjustment model pays more for members whose
medical history would indicate are expected to have higher medical costs. Under this risk adjustment
56