United Healthcare 2002 Annual Report Download - page 45
Download and view the complete annual report
Please find page 45 of the 2002 United Healthcare annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
{ 44 }
UnitedHealth Group
1DESCRIPTION OF BUSINESS
UnitedHealth Group Incorporated (also referred to as “UnitedHealth Group,” “the company,” “we,”
“us,” and “our”) is a national leader in forming and operating orderly, efficient markets for the exchange
of high quality health and well-being services. Through strategically aligned, market-defined businesses,
we offer health care access, benefits and related administrative, technology and information services
designed to enable, facilitate and advance optimal health care.
2SUMMARY OF SIGNIFICANT ACCOUNTING POLICIES
BASIS OF PRESENTATION
We have prepared the consolidated financial statements according to accounting principles generally
accepted in the United States of America and have included the accounts of UnitedHealth Group and its
subsidiaries. We have eliminated all significant intercompany balances and transactions.
USE OF ESTIMATES
These consolidated financial statements include certain amounts that are based on our best estimates
and judgments. These estimates require us to apply complex assumptions and judgments, often because
we must make estimates about the effects of matters that are inherently uncertain and will change in
subsequent periods. The most significant estimates relate to medical costs, medical costs payable,
revenues, contingent liabilities and asset valuations, allowances and impairments. We adjust these
estimates each period, as more current information becomes available. The impact of any changes in
estimates is included in the determination of earnings in the period in which the estimate is adjusted.
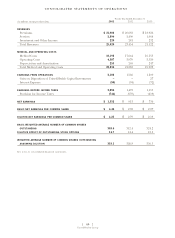
REVENUES
Premium revenues are derived from risk-based arrangements in which the premium is fixed, typically for a
one-year period, and we assume the economic risk of funding health care services and related administrative
costs. We recognize premium revenues in the period in which eligible individuals are entitled to receive
health care services. We record premium payments we receive from our customers prior to such period as
unearned premiums.
Service revenues are primarily derived from services performed for customers that self-insure the
medical costs of their employees and their dependents. Under service fee contracts, we recognize revenue
in the period the related services are performed based upon the fee charged to the customer. The
customers retain the risk of financing medical benefits for their employees and their employees’
dependents, and we administer the payment of customer funds to physicians and other health care
providers from customer-funded bank accounts. Because we do not have the obligation for funding the
medical expenses, nor do we have responsibility for delivering the medical care, we do not recognize gross
revenue and medical costs for these contracts in our consolidated financial statements.
MEDICAL COSTS AND MEDICAL COSTS PAYABLE
Medical costs include claims paid, claims processed but not yet paid, estimates for claims received but not
yet processed, and estimates for the costs of health care services eligible individuals have received under
risk-based arrangements, but for which claims have not yet been submitted.
We develop our estimates of medical costs payable using actuarial methods based upon historical
claim submission and payment data, cost trends, utilization of health care services, contracted service
rates, customer and product mix, and other relevant factors. The estimates may change as actuarial
methods change or as underlying historical data upon which estimates are based are revised with more
current information. We did not change actuarial methods during 2002, 2001 and 2000.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS