United Healthcare 2004 Annual Report Download - page 61
Download and view the complete annual report
Please find page 61 of the 2004 United Healthcare annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
UNITEDHEALTH GROUP 59
On March 15, 2000, the American Medical Association filed a lawsuit against the company in the
Supreme Court of the State of New York, County of New York. On April 13, 2000, we removed this case
to the United States District Court for the Southern District of New York. The suit alleges causes of action
based on ERISA, as well as breach of contract and the implied covenant of good faith and fair dealing,
deceptive acts and practices, and trade libel in connection with the calculation of reasonable and
customary reimbursement rates for non-network providers. The suit seeks declaratory, injunctive and
compensatory relief as well as costs, fees and interest payments. An amended complaint was filed on
August 25, 2000, which alleged two classes of plaintiffs, an ERISA class and a non-ERISA class. After the
Court dismissed certain ERISA claims and the claims brought by the American Medical Association, a
third amended complaint was filed. On October 25, 2002, the court granted in part and denied in part
our motion to dismiss the third amended complaint. On May 21, 2003, we filed a counterclaim complaint
in this matter alleging antitrust violations against the American Medical Association and asserting claims
based on improper billing practices against an individual provider plaintiff. On May 26, 2004, we filed a
motion for partial summary judgment seeking the dismissal of certain claims and parties based, in part,
due to lack of standing. On July 16, 2004, plaintiffs filed a motion for leave to file an amended complaint,
seeking to assert RICO violations.
Although the results of pending litigation are always uncertain, we do not believe the results of any
such actions currently threatened or pending, including those described above, will, individually or in
aggregate, have a material adverse effect on our consolidated financial position or results of operations.
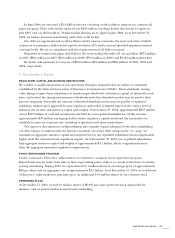
GOVERNMENT REGULATION
Our business is regulated at federal, state, local and international levels. The laws and rules governing our
business and interpretations of those laws and rules are subject to frequent change. Broad latitude is given
to the agencies administering those regulations. State legislatures and Congress continue to focus on
health care issues as the subject of proposed legislation. Existing or future laws and rules could force us
to change how we do business, restrict revenue and enrollment growth, increase our health care and
administrative costs and capital requirements, and increase our liability in federal and state courts for
coverage determinations, contract interpretation and other actions. Further, we must obtain and maintain
regulatory approvals to market many of our products.
We typically have and are currently involved in various governmental investigations, audits, and
reviews. These include routine, regular and special investigations, audits, and reviews by CMS, state
insurance and health and welfare departments and state attorneys general, the Office of the Inspector
General, the Office of Personnel Management, the Office of Civil Rights, the Department of Justice, and
U.S. Attorneys. Such government actions can result in assessment of damages, civil or criminal fines or
penalties, or other sanctions, including loss of licensure or exclusion from participation in government
programs. We record liabilities for our estimate of probable costs resulting from these matters. Although
the results of pending matters are always uncertain, we do not believe the results of any of the current
investigations, audits or reviews, currently threatened or pending, individually or in the aggregate, will
have a material adverse effect on our consolidated financial position or results of operations.