Anthem Blue Cross 2003 Annual Report Download - page 18
Download and view the complete annual report
Please find page 18 of the 2003 Anthem Blue Cross annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
page 16 ANTHEM, INC.
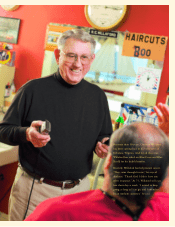
Quality
A time for innovation
Our use of innovative Web technologies allows us to serve our members, employer customers,
physicians, hospitals and brokers better than ever. Investments in www.anthem.com continue to
bring enhanced customer service, in-depth personalized health information and access to discounts
on health-related products and services to our members.
A program introduced in Virginia in 2003 gives Anthem members easy, convenient online
access to information that helps them better understand numerous medical conditions, compare how
hospitals perform in the delivery of more than 100 medical treatments and procedures and patient
safety information. This program, the Subimo Healthcare Advisor娃, will be made available nationwide
during 2004. It integrates information from a variety of objective sources and makes it readily
accessible in a user-friendly format.
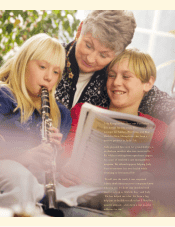
In response to the needs of an important and growing group of members, Anthem offers
MiSalud@Anthem, a Spanish-language health and wellness Web site specifically designed to assist
Spanish-speaking Anthem members. The site includes news, benefit information, health and wellness
information and a directory of physicians in Anthem’s networks.
Innovative use of technology has helped us move toward our goal of providing distinctive customer
service. Anthem receives about 475,000 claims every day, and approximately 76 percent are processed
electronically at a cost of 14 cents per claim. By contrast, it costs $2.50 each to process paper claims.
In addition to being less expensive, technology allows us to process claims faster and more accurately.
We receive about 25,000 Internet inquiries and 75,000 telephone calls daily. About a quarter of those
phone calls come through our interactive voice response telephone system, which provides members
with information quickly and conveniently in one call.