Aetna 2008 Annual Report Download
Download and view the complete annual report
Please find the complete 2008 Aetna annual report below. You can navigate through the pages in the report by either clicking on the pages listed below, or by using the keyword search tool below to find specific information within the annual report.
2008
Aetna Annual Report,
Financial Report to Shareholders
Table of contents
-
Page 1
2008 Aetna Annual Report, Financial Report to Shareholders -
Page 2
-
Page 3
...the needs of specific customer groups to create solutions that will be meaningful. In 2008, for example, Aetna offered products and services to public sector industries within Small and Middle Markets resulting in growth of 53,000 members. We opened an office in China and developed new relationships... -
Page 4
... voice in the health care debate. This year, we have chosen to move our traditional summary Annual Report to an electronic format in order to conserve resources and respect the environment. I invite you to learn more about the four essential elements of our values and how Aetna employees are helping... -
Page 5
-
Page 6
...: 2 Overview - We begin our MD&A with an overview of earnings and cash flows for the years 2006 through 2008, as well as our outlook for 2009. In this section, we also discuss significant changes to our management and Board of Directors. 5 Health Care - We provide a quantitative and qualitative... -
Page 7
...traditional and consumer-directed health insurance products and related services, including medical, pharmacy, dental, behavioral health, group life and disability plans, and medical management capabilities and health care management services for Medicaid plans. Our customers include employer groups... -
Page 8
... $1.7 billion, respectively, under share repurchase programs authorized by Aetna' s Board of Directors (the "Board") in order to return available capital to shareholders. In addition, we continue to invest in the development of our business by acquiring companies that support our strategy as well as... -
Page 9
... meaningful information about our underlying business performance. Net realized capital gains and losses arise from various types of transactions, primarily in the course of managing a portfolio of assets that support the payment of liabilities; however these transactions do not directly relate to... -
Page 10
...®, consumer-directed health plans that combine traditional POS or PPO and/or dental coverage, subject to a deductible, with an accumulating benefit account. We also offer Medicare and Medicaid products and services and specialty products, such as medical management and data analytics services... -
Page 11
... federal government are renewable for a one-year period on a calendaryear basis. We expanded our Medicare Advantage HMO and PPO offerings into select additional markets in 2008 and 2007 and now offer Medicare Advantage HMO and PPO products in 224 counties in 19 states and Washington, Annual Report... -
Page 12
...large customer' s membership from a Commercial ASC plan to a Medicare Insured plan in 2008. The increase in 2008 and 2007 was also due to increases in premiums as a result of higher membership levels, rate increases from the Centers for Medicare & Medicaid Services ("CMS") and premium rate increases... -
Page 13
...Our pharmacy benefit management services growth was due in part to an increase in Commercial pharmacy membership as well as Medicare Part D prescription drug program membership. Mail order operations reflected an increase in member utilization during this time period. GROUP INSURANCE Group Insurance... -
Page 14
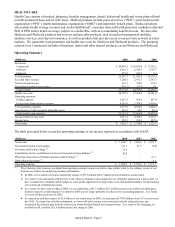
... or accept new long-term care customers, and we are working with our customers on an orderly transition of this product to other carriers. Operating Summary (Millions) Premiums: Life Disability Long-term care Total premiums Fees and other revenue Net investment income Net realized capital (losses... -
Page 15
... (refer to our discussion of Investments - Net Realized Capital Gains and Losses beginning on page 13 for additional information). Discontinued Products in Large Case Pensions Prior to 1993, we sold single-premium annuities ("SPAs") and guaranteed investment contracts ("GICs"), primarily to employer... -
Page 16
... securities in 2008. Accounting guidance requires us to recognize OTTI on these securities in order to maintain our flexibility in managing this portfolio; however, these securities continue to perform and are generating investment income to support the cash flows of our discontinued products... -
Page 17
..., of experience-rated pension contracts supported by general account assets could be withdrawn or transferred to other plan investment options at the direction of plan participants, without market value adjustment, subject to plan, contractual and income tax provisions. INVESTMENTS At December 31... -
Page 18
...operations during 2008 or 2007. Refer to Critical Accounting Estimates - Other-Than-Temporary Impairments of Investment Securities beginning on page 22 for additional information. Mortgage Loans Our mortgage loan portfolio (which is collateralized by commercial real estate) represented 10% and 8% of... -
Page 19
... sector exposure within our debt securities portfolio. In connection with our investment and risk management objectives, we also use derivative financial instruments whose market value is at least partially determined by, among other things, levels of or changes in interest rates (short-term or long... -
Page 20
... Discontinued operations Net cash provided by operating activities Cash flows from investing activities Health Care and Group Insurance Large Case Pensions Net cash used for investing activities Net cash used for financing activities Net (decrease) increase in cash and cash equivalents 2008... -
Page 21
... payments of claims to health care providers or pharmacies because certain terms of these payments are not determinable at December 31, 2008 (for example, the timing and volume of future services provided under fee-for-service arrangements and future membership levels for capitated arrangements... -
Page 22
... years for our nonqualified pension plan and our postretirement benefit plans, which we primarily fund when paid by the plans. • Deferred gains of $79.6 million related to prior cash payments which will be recognized in our earnings in the future in accordance with GAAP. • Net unrealized capital... -
Page 23
... utilization and unit costs. Changes in health care practices, inflation, new technologies, increases in the cost of prescription drugs, direct-to-consumer marketing by pharmaceutical companies, clusters of high cost cases, changes in the regulatory environment, health care provider or member fraud... -
Page 24
...we have observed an increase in our completion factors as a result of an increase in the speed of our provider claim submission and our processing times. After considering the claims paid in 2008 and 2007 with dates of service prior to the fourth quarter of the previous year, we observed the assumed... -
Page 25
... health care costs payable for benefit claims related to our Group Insurance segment. We refer to these liabilities as other insurance liabilities. These liabilities relate to our life, disability and long-term care products. Life and Disability The liabilities for our life and disability products... -
Page 26
... for life claims incurred but not yet reported to us. Long-term Care We establish a reserve for future policy benefits for our long-term care products at the time each policy is issued based on the present value of estimated future benefit payments less the present value of estimated future premiums... -
Page 27
... Moody' s Investors Service or a rating of AA or better from Standard and Poor' s). We project the benefits expected to be paid from each plan at each point in the future based on each participant' s current service (but reflecting expected future pay increases). These projected benefit payments are... -
Page 28
... for group life and disability products is recognized as revenue, net of allowances for uncollectable accounts, over the term of coverage. Amounts received before the period of coverage begins are recorded as unearned premiums. Health Care billings may be subsequently adjusted to reflect changes in... -
Page 29
... costs to us. Areas of governmental regulation include Licensure Policy forms, including plan design and disclosures Premium rates and rating methodologies Medical benefit ratios Underwriting rules and procedures Benefit mandates Market conduct Utilization review activities Annual Report - Page 24 -
Page 30
... procedures Disclosure of medical and other information In network and out-of-network provider rates of payment General assessments Provider contract forms Pharmacy and pharmacy benefit management operations Required participation in coverage arrangements for high-risk insureds, either directly... -
Page 31
... example, health care claims submission and payment, plan eligibility, precertification, claims status, plan enrollment and disenrollment, payment and remittance advice, plan premium payments and coordination of benefits). HHS also has published rules requiring the use of standardized code sets and... -
Page 32
... price fixing, group boycotts and other horizontal restraints on competition. Restricting health plan claim processing, review, payment and related procedures. Mandating internal and external grievance and appeal procedures (including expedited decision making and access to external claim review... -
Page 33
... omissions. Requiring employers to provide health care coverage for their employees. Requiring individuals to purchase health care coverage. Allowing significantly expanded access to Medicaid, Medicare, the Federal Employees Health Benefit Plan or other government-based health insurance programs, or... -
Page 34
... Medicare Advantage plans beginning in 2010, requires health plans that offer Medicare Advantage plans to have contracts with the providers their members utilize beginning in 2011, and imposes new marketing requirements for Medicare Advantage and Medicare Part D Prescription Drug plans beginning... -
Page 35
..., our Medicaid compliance efforts will continue to require significant resources. If we fail to comply with the standards, CMS may prohibit us from continuing to market and/or enroll members in one or more Medicaid products. HMO and Insurance Holding Company Laws A number of states, including... -
Page 36
... rights. Companies involved in public health care programs such as Medicare and Medicaid are often the subject of fraud and abuse investigations. The regulations and contractual requirements applicable to us and other participants in these public-sector programs are complex and subject to change... -
Page 37
... definition of disability or changing claim determination, settlement and/or payment practices, could have a material impact on our life insurance and/or disability insurance operations and/or operating results. International Regulation Certain of our Health Care operations are conducted in foreign... -
Page 38
..., general economic conditions such as inflation and employment levels, new technologies, increases in the cost of prescription drugs, direct-to-consumer marketing by pharmaceutical companies, clusters of high cost cases, changes in the regulatory environment, health care provider or member fraud and... -
Page 39
... utilization of medical and other covered services by our members and/or increases in medical unit costs, each of which would increase our costs and limit our ability to accurately detect, forecast, manage and reserve for our and our self-insured customers' medical cost trends and future health care... -
Page 40
... manage and upgrade our technology portfolio, we could, among other things, have problems determining health care cost estimates and/or establishing appropriate pricing, meeting the needs of providers, employer plan sponsors and members, or keeping pace with industry and regulatory standards... -
Page 41
...and retain membership is dependent upon providing quality customer service operations (such as call center operations, claim processing, mail order pharmacy prescription delivery, specialty pharmacy prescription delivery and customer case installation) that meet or exceed our customers' expectations... -
Page 42
... and mail order pharmacy products are more highly regulated than our Commercial products. There continues to be a heightened review by federal and state regulators of the health care insurance industry' s business and reporting practices, including utilization management, payment of providers with... -
Page 43
... Medicare PDP, mail order pharmacy, specialty pharmacy and ActiveHealth. These products subject us to regulatory and other risks that are different from the risks of providing Commercial managed care and health insurance products and may increase the risks we face from litigation, regulatory reviews... -
Page 44
... profitable membership growth, further improving the efficiency of our operations, managing certain significant technology projects, further improving relations with health care providers, negotiating contract changes with customers and providers, and implementing other business process improvements... -
Page 45
... offer new products, such as products with limited benefits, targeted at market segments, such as the uninsured, part time and hourly workers and those eligible for Medicaid, beyond those in which we traditionally have operated. Negative publicity of the health benefits industry in general or Aetna... -
Page 46
...and other quality of care and information management initiatives) lead to access by our members to quality care by providers or delivery of quality care by us would adversely affect our ability to differentiate our product and/or service offerings from those of competitors and could adversely affect... -
Page 47
...: • Health benefits provider fraud that is not prevented or detected and impacts our medical cost trends or those of our self-insured customers; • Financial loss from inadequate insurance coverage due to self insurance levels or unavailability of insurance and reinsurance coverage for credit or... -
Page 48
... per common share data) Revenue Income from continuing operations Net income Net realized capital (losses) gains, net of tax Assets Short-term debt Long-term debt Shareholders' equity Per common share data: Dividends declared Income from continuing operations: Basic Diluted Net income: Basic Diluted... -
Page 49
... and $38 million (net of pharmaceutical and processing costs of $1.6 billion, $1.4 billion and $1.4 billion) for 2008, 2007 and 2006, respectively. ** Health care costs have been reduced by fully insured member co-payments related to our mail order and specialty pharmacy operations of $111 million... -
Page 50
... Other long-term assets Separate Accounts assets (Note 2) Total assets Liabilities and shareholders' equity Current liabilities: Health care costs payable Future policy benefits Unpaid claims Unearned premiums Policyholders' funds Collateral payable under securities loan agreements Short-term debt... -
Page 51
... to initially recognize the funded status of pension and OPEB plans Common shares issued for benefit plans, including tax benefit Repurchases of common shares Dividends declared ($.04 per share) Balance at December 31, 2006 Cumulative effect of new accounting standards Beginning balance at January... -
Page 52
... Net issuance of short-term debt Repayment of long-term debt Deposits and interest credited for investment contracts Withdrawals of investment contracts Common shares issued under benefit plans Stock-based compensation tax benefits Common shares repurchased Dividends paid to shareholders Net cash... -
Page 53
...®, consumer-directed health plans that combine traditional POS or PPO and/or dental coverage, subject to a deductible, with an accumulating benefit account (which may be funded by the plan sponsor and/or the member in the case of HSAs). We also offer Medicare and Medicaid products and services and... -
Page 54
...In February 2008, the Financial Accounting Standards Board ("FASB") released FASB Staff Position No. FAS 157-2, "Effective Date of FASB Statement No. 157," which delays the effective date of FAS 157 for nonfinancial assets and liabilities until January 2009. Refer to Note 15 beginning on page 72 for... -
Page 55
... terms. Interest income on problem loans is recognized on a cash basis. Cash payments on loans in the process of foreclosure are treated as a return of principal. Mortgage loans with a maturity date or a committed prepayment date of less than one year from the balance sheet date are reported... -
Page 56
... the ability to meet their obligations. In the normal course of business, we enter into agreements with other insurance companies under which we assume reinsurance, primarily related to our group life and health products (refer to Note 17 beginning on page 75 for additional information). We do not... -
Page 57
...unpaid fee-for-service medical, dental and pharmacy claims, capitation costs and other amounts due to health care providers pursuant to risk-sharing arrangements related to Health Care' s POS, PPO, HMO, Indemnity, Medicare and Medicaid products. Unpaid health care claims include Annual Report - Page... -
Page 58
... claims experience under the contracts through the balance sheet date. Future policy benefits Future policy benefits consist primarily of reserves for limited payment pension and annuity contracts in the Large Case Pensions business and long-duration group life and long-term care insurance contracts... -
Page 59
... amounts. Other premium revenue for group life, long-term care and disability products is recognized as income, net of allowances for termination and uncollectable accounts, over the term of the coverage. Other premium revenue for Large Case Pensions' limited payment pension and annuity contracts is... -
Page 60
... Act expanded Medicare, primarily by adding a voluntary prescription drug benefit for Medicare eligible individuals beginning in 2006. We were selected by the Centers for Medicare & Medicaid Services ("CMS") to be a national provider of PDP in all 50 states to both individuals and employer groups in... -
Page 61
... severance and facility charge related to actions taken. This charge is reflected in total general and administrative expenses. Refer to the reconciliation of operating earnings to income from continuing operations in Note 19 beginning on page 79 for additional information. Annual Report - Page 56 -
Page 62
... Health care costs payable, beginning of the period - net Acquisition of businesses Add: Components of incurred health care costs Current year Prior years (1) Total incurred health care costs Less: Claims paid Current year Prior years Total claims paid Health care costs payable, end of period - net... -
Page 63
... that support our experience-rated and discontinued products at December 31, 2007. Changes in net unrealized capital gains (losses) on these securities are not reflected in accumulated other comprehensive loss. Refer to Note 2 beginning on page 48 for additional information. Annual Report - Page... -
Page 64
...one year are classified as long-term investments on our consolidated balance sheets. When a debt or equity security is in an unrealized capital loss position, we monitor the duration and severity of the loss to determine if sufficient market recovery can occur within a reasonable period of time. We... -
Page 65
... 2007 were generally caused by the widening of credit spreads relative to the interest rates on U.S. Treasury securities and an increase in interest rates on U.S. Treasury securities. Mortgage Loans Our mortgage loans are secured by commercial real estate. We had no material problem, restructured or... -
Page 66
... income to support the needs of our businesses. However, accounting guidance requires us to assert our intent and ability to hold such securities until market recovery to avoid loss recognition. In order to maintain appropriate flexibility in managing our investment portfolio, we do not make... -
Page 67
...) Net derivative gains ($24.9 pretax) Pension liability adjustment ($8.8 pretax) Reclassification to earnings ($(15.7) pretax) Adjustment to initially recognize the funded status of pension and OPEB plans Balance at December 31, 2006 Effect of changing measurement date of pension and OPEB plans... -
Page 68
...23.9 3.1 13.4 (1.4) 12.0 OPEB Plans Unrecognized Unrecognized Net Actuarial Prior Service Losses Costs $ (75.8) $ 36.7 $ (1.6) (77.4) 26.9 3.4 (47.1) (10.2) 1.7 (55.6) (.6) 36.1 (Millions) Balance at December 31, 2006 Effect of changing measurement date of pension and OPEB plans pursuant to FAS 158... -
Page 69
... those of our former parent company. For certain of our employees, we provide a noncontributory, defined benefit pension plan, the Aetna Pension Plan, which is a tax-qualified pension plan. All pension plan participants accrue future benefits under a cash balance formula. Annual Report - Page 64 -
Page 70
... balance accounts and the plan may continue to be used to credit special pension arrangements. In addition, we currently provide certain medical and life insurance benefits for retired employees, including those of our former parent company. We provide subsidized health benefits to certain eligible... -
Page 71
... and ending balances of the fair value of plan assets during 2008 and 2007 for the pension and OPEB plans: (Millions) Fair value of plan assets, beginning of year Net effect of changing measurement date pursuant to FAS 158 Actual (loss) return on plan assets Employer contributions Benefits paid Fair... -
Page 72
... improve portfolio and operational risk characteristics. Public and private equity investments are used primarily to increase overall plan returns. Real estate investments are viewed favorably for their diversification benefits and above-average dividend generation. Fixed income investments provide... -
Page 73
... plans represent payments to retirees for current benefits. We have no plans to return any pension or OPEB plan assets to the Company in 2009. Expected benefit payments, which reflect future employee service, as appropriate, of the pension and OPEB plans to be paid for each of the next five years... -
Page 74
...of stock options and SARs vested 2008 2007 $ 29.7 $ 163.1 75.5 494.1 26.4 172.9 86.5 18.0 2006 $ 105.8 309.2 108.2 71.0 We settle employee stock options with newly issued common stock and generally utilize the proceeds to repurchase common stock in the open market in the same period. Annual Report... -
Page 75
... SARs outstanding and exercisable at December 31, 2008 (number of stock options and SARs and aggregate intrinsic values in millions): Outstanding Weighted Average Weighted Remaining Average Aggregate Contractual Exercise Intrinsic Life (Years) Price Value 2.1 $ 7.95 $ 154.8 3.8 14.52 190.8 9.0 22.59... -
Page 76
...the Board declared an annual cash dividend of $.04 per common share to shareholders of record at the close of business on November 13, 2008. The $18 million dividend was paid on November 28, 2008. In addition to the capital stock disclosed on our balance sheets, we have authorized 7.6 million shares... -
Page 77
... of equity securities: those that are publicly traded and those that are privately held. Our publicly traded securities are classified as Level 1 because quoted prices are available for these securities in an active market. For privately held equity securities, there is no Annual Report - Page 72 -
Page 78
... Balance Total $ 681.3 (51.9) (31.2) (19.0) (83.1) (11.1) $ 485.0 $ $ Amount of Level 3 net unrealized capital losses included in net income $ (53.8) $ $ (53.8) Reflects realized and unrealized capital gains and losses on investments supporting our experience-rated and discontinued products... -
Page 79
... Long-term debt 39.1 525.6 3,638.3 38.0 428.8 3,372.2 70.8 546.9 3,138.5 71.8 502.3 3,193.8 Separate Accounts Measured at Fair Value in our Balance Sheets Separate Account assets in Large Case Pensions represent funds maintained to meet specific objectives of contract holders. Since contract... -
Page 80
... obligations related to paid-up group whole life insurance. Effective October 1, 1998, we reinsured certain policyholder liabilities and obligations related to individual life insurance (in conjunction with our former parent company' s sale of this business). These transactions were in the form of... -
Page 81
.... Effective October 1, 2008, we entered into an agreement with Hannover Life Reassurance Company of America to reinsure fifty percent of our group term life and group accidental death and dismemberment insurance policies. We entered into this contract in order to reduce the risk on catastrophic loss... -
Page 82
...of our health insurance plans that pay benefits to members who receive services from out-of-network providers. The plaintiff seeks actual damages, treble and other punitive damages, and injunctive relief, plus costs and attorneys' fees. This case is similar to other actions pending in the New Jersey... -
Page 83
...those benefit plans that employ a reasonable and customary standard for out-ofnetwork reimbursements. In February 2009, Aetna agreed with the New York Attorney General and the Texas Attorney General to reimburse college student members for approximately $5 million of claims relating to care rendered... -
Page 84
... processing, information privacy, provider network structure (including the use of performance-based networks), delegated arrangements, pharmacy benefit management practices and claim payment practices (including payments to out-of-network providers). As a leading national health care benefits... -
Page 85
...charge to net income, reflected in general and administrative expenses in 2006. Revenues from external customers by product in 2008, 2007 and 2006 were as follows: (Millions) Health care premiums Health care fees and other revenue Group life Group disability Group long-term care Large case pensions... -
Page 86
... supporting these products and the cash flows expected to be required to meet the obligations of the outstanding contracts. Because we projected anticipated cash shortfalls in our discontinued products, at the time of discontinuance we established a receivable from Large Case Pensions' continuing... -
Page 87
... result of sales. The resulting proceeds were primarily reinvested in debt and equity securities. Over time, the then existing mortgage loan and real estate portfolios and the reinvested proceeds have resulted in greater investment returns than we originally assumed in 1993. Annual Report - Page 82 -
Page 88
... liabilities in 2008, 2007 and 2006 were as follows: (Millions) Scheduled contract maturities, settlements and benefit payments Participant-directed withdrawals $ 2008 454.3 .1 $ 2007 468.0 .3 $ 2006 481.0 .4 Cash required to fund these distributions was provided by earnings and scheduled payments... -
Page 89
...' s Board of Directors engages KPMG LLP, an independent registered public accounting firm, to audit our consolidated financial statements and express their opinion thereon. Members of that firm also have the right of full access to each member of management in conducting their audits. The report of... -
Page 90
... Plaza Hartford, CT 06103-4103 Report of Independent Registered Public Accounting Firm The Board of Directors and Shareholders Aetna Inc. We have audited the accompanying consolidated balance sheets of Aetna Inc. and subsidiaries (the "Company") as of December 31, 2008 and 2007, and the related... -
Page 91
... cash flows for each of the years in the three-year period ended December 31, 2008, in conformity with accounting principles generally accepted in the United States of America. Also in our opinion, the Company maintained, in all material respects, effective internal control over financial reporting... -
Page 92
... companies included in the MSHPI were: Aetna Inc., Amerigroup Corporation, Centene Corporation, CIGNA Corporation, Coventry Health Care, Inc., Health Net, Inc., Humana Inc., Molina Healthcare, Inc., UnitedHealth Group Incorporated, Wellcare Health Plans Inc. and Wellpoint, Inc. Shareholder returns... -
Page 93
... Thomson Reuters Foundation Edward J. Ludwig Chairman of the Board and Chief Executive Officer Becton, Dickinson and Company Joseph P. Newhouse John D. MacArthur Professor of Health Policy and Management Harvard University Ronald A. Williams Chairman and Chief Executive Officer Aetna Inc. Executive... -
Page 94
...The annual meeting of shareholders of Aetna Inc. ("Aetna" or the "Company") will be held on Friday, May 29, 2009, at the Omni Jacksonville Hotel in Jacksonville, Florida. Corporate Headquarters 151 Farmington Avenue Hartford, CT 06156 Phone: 860-273-0123 Stock Exchange Listing Aetna' s common shares... -
Page 95
...and related regulations, are filed as exhibits to the 2008 Form 10-K. In addition, NYSE regulations require that the Chief Executive Officer provide the NYSE each year with a certification of compliance with the NYSE' s corporate governance listing standards following the annual shareholders meeting... -
Page 96
... Aetna employee and own shares in the Company' s 401(k) Plan, you can enroll by visiting www.computershare.com/econsent Other Shareholder Inquiries Office of the Corporate Secretary Aetna Inc. 151 Farmington Avenue, RW61 Hartford, CT 06156-3215 Fax: 860-293-1361 E-mail address: ShareholderRelations... -
Page 97
-
Page 98
www.aetna.com